No products in the cart.
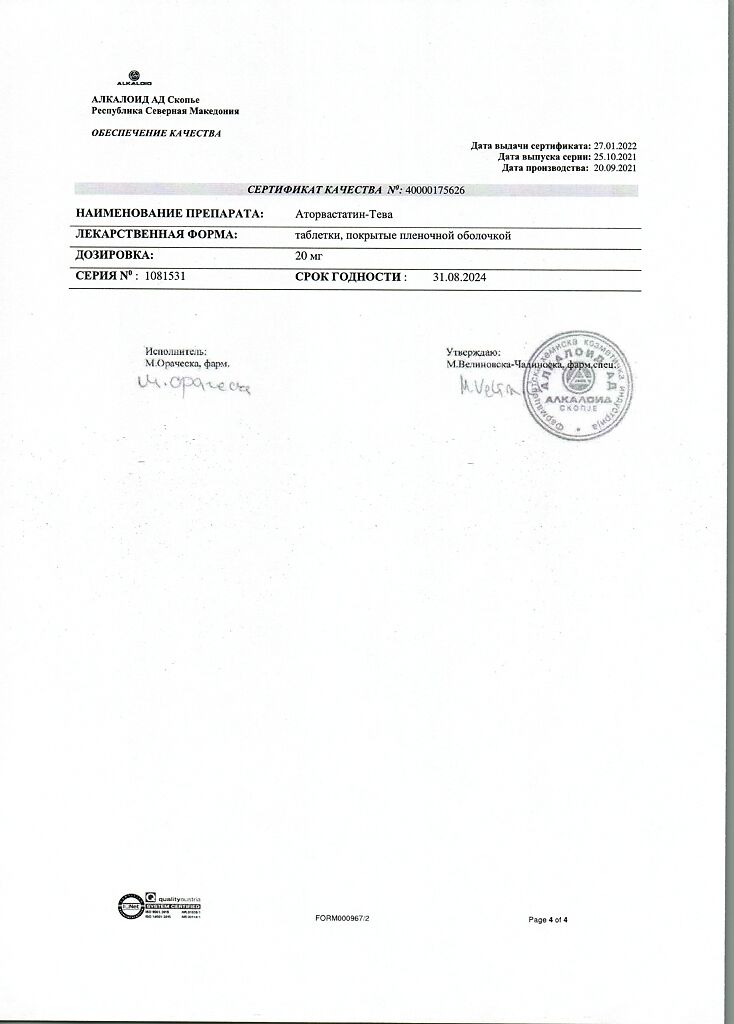
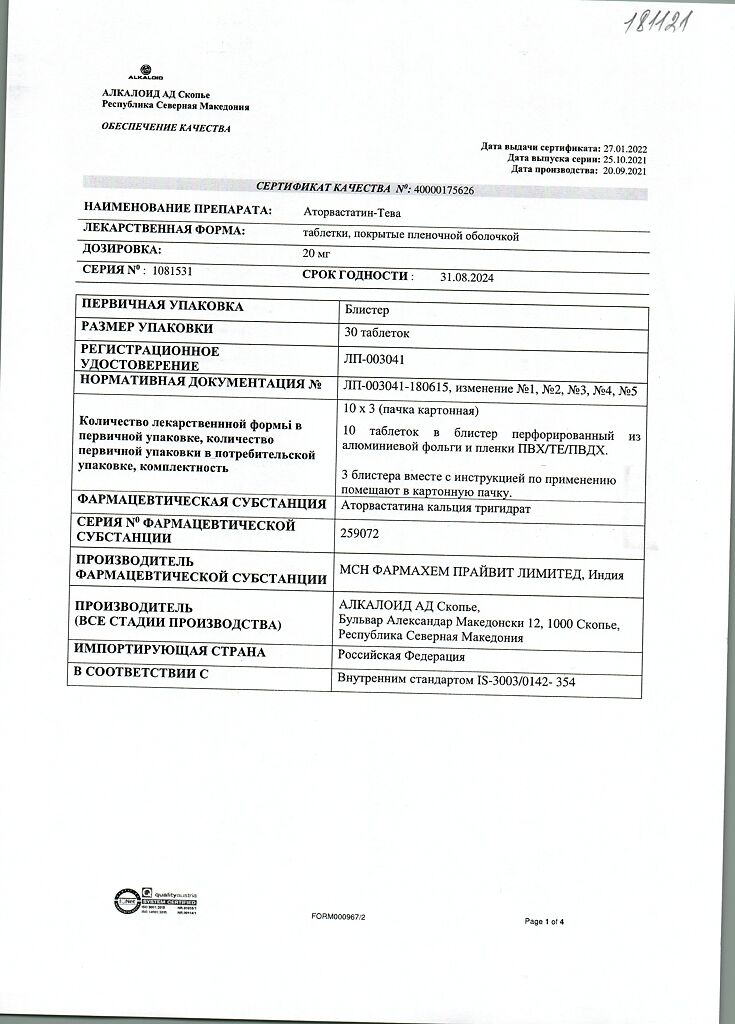
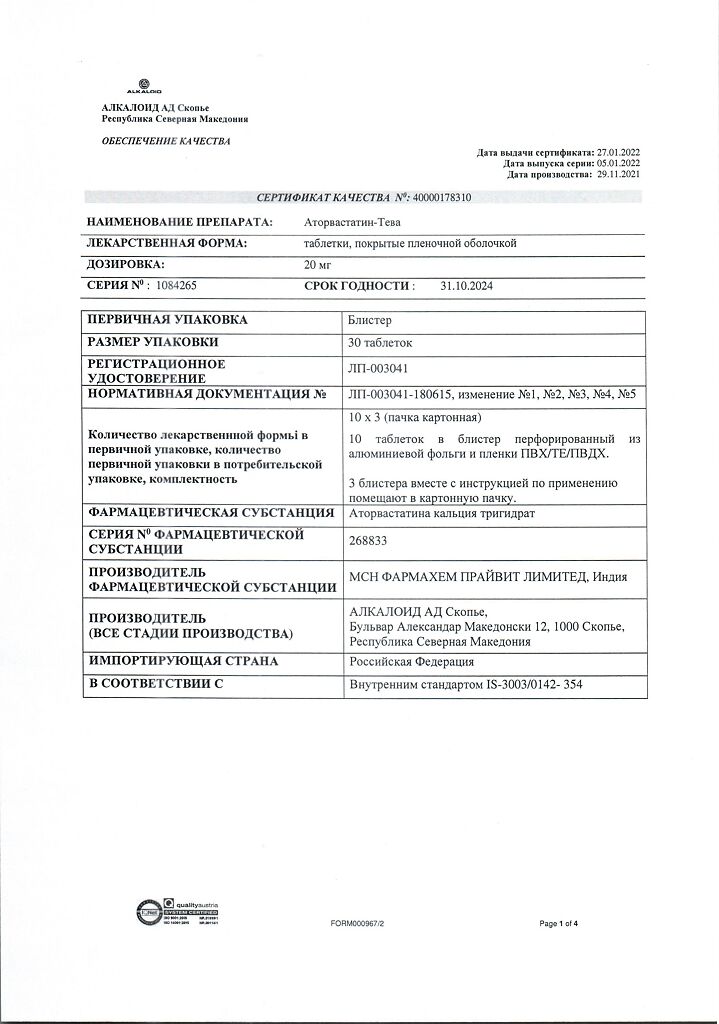
Atorvastatin-Teva, 20 mg 30 pcs
€10.41 €9.11
Description
Pharmacotherapeutic group: hypolipidemic drug – HMG-CoA reductase inhibitor
ATC code: C10AA05.
Pharmacological properties
Pharmacodynamics
Atorvastatin is a selective competitive inhibitor of HMG-CoA reductase, the enzyme that determines the marginal rate of cholesterol biosynthesis, responsible for converting 3-hydroxy-3-methyl-glutaryl-coenzyme A to mevalonate, a precursor of sterols, including cholesterol. In the liver, triglycerides and cholesterol are incorporated into very low density lipoproteins (VLDL), entering the blood plasma and being transported to peripheral tissues. Low-density lipoproteins (LDL) are formed from LDL, which are catabolized mainly through interaction with high-affinity LDL receptors.
Atorvastatin reduces plasma levels of cholesterol and lipoproteins by inhibiting HMG-CoA reductase and cholesterol synthesis in the liver and by increasing the number of “hepatic” LDL receptors on the cell surface, increasing LDL capture and catabolism.
Atorvastatin reduces LDL production and LDL particles. Atorvastatin causes a marked and persistent increase in LDL receptor activity in combination with favorable changes in the quality of circulating LDL particles.
Dose-dependently reduces LDL levels in patients with homozygous hereditary hypercholesterolemia who are resistant to therapy with other hypolipidemic agents.
Dose/effect studies have shown that atorvastatin reduces total cholesterol (by 30-46%), LDL cholesterol (by 41-61%), apolipoprotein B (by 34-50%) and triglycerides (by 14-33%), while causing, to varying degrees, increases in HDL cholesterol and apolipoprotein A levels. These results were similar in patients with heterozygous familial hypercholesterolemia, nonfamilial forms of hypercholesterolemia, and mixed hyperlipidemia, including patients with insulin-independent diabetes.
The risk of cardiovascular disease and, therefore, the risk of death are reduced due to decreased levels of total cholesterol, LDL cholesterol and apolipoprotein B. Studies on the effect of atorvastatin on cardiovascular morbidity and mortality have not yet been completed.
There have been no differences in safety, efficacy or achievement of hypolipidemic therapy goals in elderly patients compared to the general population when using the drug.
Pharmacokinetics
Intake. Atorvastatin is rapidly absorbed into the blood after oral administration. Maximal concentration (Сmax) in plasma is reached within 1-2 hours, Сmax in women is 20% higher, area on curve “concentration-time” (AUC) is 10% lower; Сmax in patients with alcoholic liver cirrhosis is 16 times higher, AUC – 11 times higher. Food intake slightly reduces speed and duration of drug absorption (by 25% and 9% respectively), but cholesterol decrease is similar to that of atorvastatin without food. Absolute bioavailability of atorvastatin is approximately 12%, systemic bioavailability determining inhibitory activity against HMG-CoA reductase – 30%. Low systemic bioavailability is due to presystemic metabolism in the gastrointestinal mucosa and during “first passage” through the liver.
Distribution. The mean volume of distribution of atorvastatin is approximately 381 liters. The binding to plasma proteins is 98%.
Metabolism. Elimation. Atorvastatin is excreted predominantly with bile after hepatic and/or extrahepatic metabolism (it is not subjected to marked intestinal-hepatic recirculation). The elimination half-life is 14 hours. Inhibitory activity against HMG-CoA reductase lasts about 20-30 hours due to the presence of active metabolites. Less than 2% of the oral dose is detected in the urine. It is not excreted during hemodialysis.
Indications
Indications
in patients with primary hypercholesterolemia, heterozygous familial and non-familial hypercholesterolemia and combined (mixed) hyperlipidemia (Fredrickson types IIa and IIb) in combination with diet to reduce elevated levels of total cholesterol, LDL cholesterol, apolipoprotein B and triglycerides and increase HDL cholesterol levels;
for the treatment of patients with elevated serum triglyceride levels (Fredrickson type IV) and patients with dysbetalipoproteinemia (Fredrickson type III) in whom diet therapy does not provide an adequate effect;
in patients with homozygous familial hypercholesterolemia to reduce total and LDL cholesterol levels when diet therapy and other non-pharmacological treatments are not effective enough.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: lipid-lowering agent – HMG-CoA reductase inhibitor
ATX code: C10AA05.
Pharmacological properties
Pharmacodynamics
Atorvastatin is a selective competitive inhibitor of HMG-CoA reductase, an enzyme that determines the maximum rate of cholesterol biosynthesis, responsible for the conversion of 3-hydroxy-3-methyl-glutaryl coenzyme A to mevalonate, a precursor of sterols, including cholesterol. In the liver, triglycerides and cholesterol are incorporated into very low-density lipoproteins (VLDL), enter the blood plasma and are transported to peripheral tissues. VLDL produces low-density lipoproteins (LDL), which are catabolized primarily through interaction with high-affinity LDL receptors.
Atorvastatin reduces cholesterol and lipoprotein levels in the blood plasma by inhibiting HMG-CoA reductase and cholesterol synthesis in the liver, as well as by increasing the number of “liver” LDL receptors on the cell surface, increasing the uptake and catabolism of LDL.
Atorvastatin reduces LDL production and the number of LDL particles. Atorvastatin causes a marked and persistent increase in LDL receptor activity combined with favorable changes in the quality of circulating LDL particles.
Dose-dependently reduces LDL levels in patients with homozygous hereditary hypercholesterolemia, resistant to therapy with other lipid-lowering drugs.
Dose-response studies have shown that atorvastatin reduces total cholesterol (by 30-46%), LDL cholesterol (by 41-61%), apolipoprotein B (by 34-50%), and triglycerides (by 14-33%), while causing, to varying degrees, increases in HDL cholesterol and apolipoprotein A. These results were similar in patients with heterozygous familial hypercholesterolemia, non-familial forms of hypercholesterolemia and mixed hyperlipidemia, including patients with non-insulin-dependent diabetes mellitus.
Due to the reduction in total cholesterol, LDL cholesterol and apolipoprotein B, the risk of cardiovascular disease is reduced and, accordingly, the risk of death is reduced. Studies of the effect of atorvastatin on cardiovascular morbidity and mortality have not yet been completed.
When using the drug in elderly patients, there were no differences in safety, effectiveness, or achievement of lipid-lowering therapy goals compared to the general population.
Pharmacokinetics
Suction. After oral administration, atorvastatin is rapidly absorbed into the blood. The maximum concentration (Cmax) in the blood plasma is achieved within 1-2 hours, Cmax in women is 20% higher, the area along the concentration-time curve (AUC) is 10% lower; Cmax in patients with alcoholic cirrhosis of the liver increases 16 times, AUC – 11 times. Eating slightly reduces the rate and duration of drug absorption (by 25% and 9%, respectively), but the reduction in cholesterol is similar to that when taking atorvastatin without food. The absolute bioavailability of atorvastatin is approximately 12%, systemic bioavailability, which determines the inhibitory activity against HMG-CoA reductase, is 30%. Low systemic bioavailability is due to first-pass metabolism in the gastrointestinal mucosa and during the “first pass” through the liver.
Distribution. The mean volume of distribution of atorvastatin is approximately 381 L. Communication with blood plasma proteins – 98%.
Metabolism. Atorvastatin is metabolized primarily in the liver with the participation of cytochrome P450 isoenzymes CYP3A4, CYP3A5 and CYP3A7 with the formation of pharmacologically active metabolites (ortho- and parahydroxylated derivatives, beta-oxidation products). In vitro, ortho- and parahydroxylated metabolites have an inhibitory effect on HMG-CoA reductase comparable to that of atorvastatin. The inhibitory effect of the drug on HMG-CoA reductase is approximately 70% determined by the activity of circulating metabolites.
Excretion. Atorvastatin is excreted primarily in bile after hepatic and/or extrahepatic metabolism (it does not undergo significant enterohepatic recirculation).
The half-life is 14 hours. Inhibitory activity against HMG-CoA reductase lasts about 20-30 hours due to the presence of active metabolites. Less than 2% of the dose taken orally is determined in the urine. It is not excreted during hemodialysis.
Special instructions
Special instructions
Before using the drug Atorvastatin-Teva, the patient must begin to follow a standard cholesterol-lowering diet, which he must follow during the entire treatment period.
The use of HMG-CoA reductase inhibitors to reduce the concentration of lipids in the blood can lead to changes in biochemical parameters reflecting the functional state of the liver. Liver function should be monitored before starting therapy, 6 weeks, 12 weeks after starting atorvastatin, and after each dose increase, and periodically, such as every 6 months. An increase in the activity of hepatic transaminases in the blood serum may be observed during therapy with Atorvastatin-Teva. Patients who experience increased activity of liver transaminases should be monitored until their activity decreases. In the case of a persistent increase in the activity of “liver” transaminases to a level exceeding the ULN by more than 3 times, it is recommended to reduce the dose of Atorvastatin-Teva or discontinue treatment.
Atorvastatin-Teva should be used with caution in patients who abuse alcohol and/or have a history of liver disease. Active liver disease or a persistent increase in the activity of liver transaminases of unknown origin are contraindications to the use of Atorvastatin-Teva.
Treatment with Atorvastatin-Teva, like other HMG-CoA reductase inhibitors, can cause myopathy. The diagnosis of myopathy should be considered in patients with widespread myalgia or muscle weakness and/or a marked increase in CPK activity (more than 10 times the ULN). Patients should be warned to immediately notify their physician if they experience unexplained muscle pain or weakness if accompanied by malaise or fever. Therapy with Atorvastatin-Teva should not be started if the CPK level is initially elevated 5 times higher than the ULN (it is recommended to repeat the analysis after 5-7 days). During therapy, if CPK increases to more than 5 times the ULN or in the presence of confirmed or suspected myopathy, it is necessary to interrupt the use of Atorvastatin-Teva with the possible resumption of the drug if CPK activity decreases. The risk of developing myopathy during treatment with other drugs in this class increased with simultaneous use of cyclosporine, clarithromycin, delavirdine, stripentol, ketoconazole, itraconazole, protease inhibitors, fibrates, erythromycin, niacin, or azole antifungals. If the patient receives therapy with these drugs or there is a need for their use, a dose adjustment of Atorvastatin-Teva is required.
The simultaneous use of Atorvastatin-Teva and fusidic acid is not recommended. If the use of fusidic acid is necessary, therapy with Atorvastatin-Teva should be temporarily discontinued.
CPK activity before starting therapy with Atorvastatin-Teva is subject to mandatory determination in patients with renal failure, hypothyroidism, congenital diseases of skeletal muscles, manifestations of toxicity when using statins or fibrates, a history of liver disease, alcoholism, and over the age of 70 years.
When using Atorvastatin-Teva in combination with fibrates, erythromycin, immunosuppressive agents, azole antifungals or nicotinic acid in lipid-lowering doses (more than 1 g per day), the possible risks and expected benefits of treatment should be carefully assessed. During therapy with Atorvastatin-Teva, it is necessary to monitor the appearance of patient complaints of pain or muscle weakness, especially during the first months of treatment and during periods of increasing the dose of any drug. In such situations, periodic determination of CPK activity is recommended.
When using the drug Atorvastatin-Teva, as well as other drugs of this class, cases of rhabdomyolysis with acute renal failure caused by myoglobinuria have been described. Therapy with Atorvastatin-Teva should be temporarily discontinued or completely discontinued if signs of myopathy appear or if there is a risk factor for the development of renal failure due to rhabdomyolysis (for example, severe acute infection, hypotension, major surgery and trauma, severe metabolic, endocrine and electrolyte disturbances, uncontrolled seizures).
There are reports of the development of interstitial lung disease (ILD) in patients receiving statin therapy for a long time, manifested by cough, shortness of breath and deterioration in general condition. If ILD develops, therapy with Atorvastatin-Teva should be discontinued.
Impact on the ability to drive vehicles and machinery
No adverse effects of atorvastatin on the ability to drive or use machines have been reported.
Active ingredient
Active ingredient
Atorvastatin
Composition
Composition
1 tablet contains:
active ingredient atorvastatin calcium (in terms of atorvastatin) 10.36 mg (10 mg) / 20.72 mg (20 mg) / 41.44 mg (40 mg) / 82.88 mg (80 mg); excipients: lactose monohydrate 94.94/189.88/379.76/759.52 mg; povidone K-30 4.00/8.00/16.00/32.00 mg; Eudragit E100 (butyl methacrylate, dimethylaminoethyl methacrylate and methyl methacrylate copolymer 1:2:1) 1.50/3.00/6.00/12.00 mg; alpha-tocopherol macrogol succinate 3.00/6.00/12.00/24.00 mg; croscarmellose sodium 5.00/10.00/20.00/40.00 mg; sodium stearyl fumarate 1.20/2.40/4.80/9.60 mg; Opadry YS-1R-7003 (titanium dioxide 0.9375/1.8750/3.7500/7.500 mg; hypromelose-2910 3cP (E464) 0.8963/1.7926/3.5852/7.1704 mg; hypromelose-2910 5cP (E464) 0.8963/1.7926/3.5852/7.1704 mg; macrogol-400 0.240/0.480/0.960/1.920 mg; polysorbate-80 0.030/0.060/0.120/0.240 mg).
Pregnancy
Pregnancy
Atorvastatin is contraindicated for use during pregnancy and breastfeeding.
It is not known whether atorvastatin is excreted in breast milk. Considering the possibility of adverse events in infants, if it is necessary to use the drug during lactation, the issue of stopping breastfeeding should be decided.
Women of reproductive age should use adequate contraception during treatment. Atorvastatin should only be prescribed to women of reproductive age if the likelihood of pregnancy is very low and the patient is informed of the possible risk of treatment to the fetus.
Contraindications
Contraindications
Hypersensitivity to the components of the drug;
active liver disease or increased activity of liver enzymes of unknown origin (more than 3 times the upper limit of normal);
liver failure (severity according to Child-Pugh classification A and B);
pregnancy;
breastfeeding period;
age under 18 years (efficacy and safety have not been established);
lactose intolerance, lactase deficiency, glucose-galactose malabsorption syndrome.
With caution
Alcohol abuse, history of liver disease, severe electrolyte imbalance, endocrine and metabolic disorders, arterial hypotension, severe acute infections (sepsis), uncontrolled epilepsy, major surgery, trauma, skeletal muscle diseases.
Side Effects
Side Effects
The incidence of side effects is classified according to the recommendations of the World Health Organization: very often – at least 10%; often – at least 1%, but less than 10%; infrequently – not less than 0.1%, but less than 1%; rarely – not less than 0.01%, but less than 0.1%; very rarely (including isolated cases) – less than 0.01%; frequency unknown – adverse reactions with unknown frequency.
From the blood and lymphatic system: rarely – thrombocytopenia.
From the immune system: often – an allergic reaction; very rarely – angioedema; anaphylactic shock.
From the nervous system: often – headache; infrequently – dizziness, paresthesia, hypoesthesia, amnesia, disturbance of taste, insomnia, nightmares; rarely – peripheral neuropathy; frequency unknown – depression, memory loss or decline, depression, sleep disturbance.
From the side of the organ of vision: infrequently – decreased clarity of vision; rarely – visual impairment.
From the organ of hearing and labyrinthine disorders: infrequently – “noise” in the ears, very rarely – hearing loss.
From the respiratory system, chest organs and mediastinum: often – nasopharyngitis, nosebleeds, pain in the pharyngo-laryngeal region; frequency unknown – interstitial lung diseases.
From the gastrointestinal tract: often – nausea, flatulence, constipation, dyspepsia, diarrhea; infrequently – belching, vomiting, abdominal pain, pancreatitis.
From the liver and biliary tract: infrequently – hepatitis; rarely – cholestasis; very rarely – liver failure.
From the skin and subcutaneous tissues: infrequently – alopecia, skin rash, itching, urticaria; rarely – bullous dermatitis, erythema multiforme; very rarely – Stevens-Johnson syndrome, toxic epidermal necrolysis.
From the musculoskeletal system and connective tissue: often – myalgia, arthralgia, pain in the extremities, muscle spasm, back pain, swelling in the joints; uncommon – neck pain, muscle weakness; rarely – myopathy, myositis, rhabdomyolysis, tendinopathy complicated by tendon rupture; frequency unknown – immune-mediated necrotizing myopathy.
From the reproductive system: very rarely – gynecomastia; frequency unknown – sexual dysfunction.
General disorders: uncommon – asthenia, weakness, chest pain, peripheral edema, increased body temperature, lethargy, weight gain, anorexia.
Laboratory indicators: often – hyperglycemia, increased creatine kinase activity in the blood serum; infrequently – leukocyturia, hypoglycemia, increased activity of “liver” transaminases; frequency unknown – increased concentration of glycosylated hemoglobin.
Interaction
Interaction
Effect of drugs on the effects of atorvastatin
The risk of myopathy during treatment with HMG-CoA reductase inhibitors increases when used concomitantly with cyclosporine, fibrates, macrolides (including erythromycin), azole antifungals or nicotinic acid.
In some rare cases, these combinations may cause rhabdomyolysis, accompanied by renal failure. In this regard, a careful assessment of the ratio of possible risks and expected benefits of combination treatment is necessary (see section “Special instructions”).
CYP3A4 isoenzyme inhibitors
Atorvastatin is metabolized with the participation of the CYP3A4 isoenzyme. When atorvastatin is used concomitantly with inhibitors of the CYP3A4 isoenzyme (for example, cyclosporine, macrolide antibiotics, for example, erythromycin and clarithromycin, nefazodone, azole antifungals, for example, itraconazole, and HIV protease inhibitors), drug interactions may occur. With the combined use of drugs, increased concentrations of atorvastatin in the blood plasma may be observed.
Concomitant use with drugs that reduce the concentration of endogenous steroid hormones (including cimetidine, ketoconazole, spironolactone) increases the risk of a decrease in endogenous steroid hormones.
OATP1B1 transport protein inhibitors
Atorvastatin and its metabolites are substrates for the transport protein OATP1B1. Inhibitors of the transport protein OATP1B1 (for example, cyclosporine) may increase the bioavailability of atorvastatin.
Itraconazole
With simultaneous use of atorvastatin and itraconazole, an increase in AUC was found to be three times higher than normal.
Protease inhibitors
The simultaneous use of atorvastatin with protease inhibitors, known as inhibitors of the CYP3A4 isoenzyme, was accompanied by an increase in the concentration of atorvastatin in the blood plasma.
Grapefruit juice
Grapefruit juice contains at least one ingredient that is a CYP3A4 inhibitor and may cause increased plasma concentrations of drugs metabolized by CYP3A4. Daily consumption of 240 ml of grapefruit juice increased the AUC of atorvastatin by 37% and decreased the AUC of the active orthohydroxy metabolite by 20.4%. Consumption of large amounts of grapefruit juice (more than 1.2 liters per day for 5 days) increased the AUC of atorvastatin by 2.5 times, and the AUC of active HMG-CoA reductase inhibitors (atorvastatin + its metabolites) by 1.3 times. In this regard, consumption of large quantities of grapefruit juice during treatment with atorvastatin is not recommended.
Inducers of the CYP3A4 isoenzyme
The simultaneous use of atorvastatin with drugs that induce the CYP3A4 isoenzyme (rifampicin, phenazone, efavirenz, St. John’s wort preparations) can significantly reduce the concentration of atorvastatin in the blood plasma. The mechanism of interaction with atorvastatin and other substrates of the CYP3A4 isoenzyme is unknown; however, the possibility of these interactions should be taken into account when using drugs with a low therapeutic index – in particular, class III antiarrhythmic drugs, for example, amiodarone.
Ezetemibe, fusidic acid
With simultaneous use, the risk of adverse effects from the musculoskeletal system, including rhabdomyolysis, increases.
Gemfibrozil/fibrates
The risk of atorvastatin-induced myopathy may be increased when used concomitantly with fibrates. In vitro studies suggest that gemfibrozil may also interact with atorvastatin by inhibiting its glucuronidation, which may cause increased plasma concentrations of atorvastatin (see Precautions).
Colestipol
When used concomitantly with colestipol, a decrease in plasma concentrations of atorvastatin by approximately 25% was observed. However, when atorvastatin and colestipol were used in combination, the effects on lipids were greater than when either drug was used alone.
Antacids
With simultaneous oral administration of atorvastatin and a suspension containing magnesium and aluminum hydroxide, the concentration of atorvastatin in the blood plasma decreased by approximately 35%; however, LDL concentration did not change.
Phenazone
With simultaneous use, atorvastatin does not affect the pharmacokinetics of phenazone, so it can be assumed that interaction with other drugs that are metabolized by the same cytochrome P450 isoenzymes is not expected.
Cimetidine
A study of the simultaneous use of cimetidine and atorvastatin did not reveal a significant interaction between these drugs.
Amlodipine
With simultaneous use of 80 mg of atorvastatin and 10 mg of amlodipine, no changes in atorvastatin at steady state were detected.
Others
There were no clinically significant adverse interactions between atorvastatin and antihypertensive drugs.
Atorvastatin did not have a clinically significant effect on the plasma concentration of terfenadine, which is metabolized by the CYP3A4 isoenzyme. In this regard, it seems unlikely that atorvastatin can significantly affect the pharmacokinetic parameters of other drugs that are metabolized by the CYP3A4 isoenzyme.
Table 1. Effect of drugs on the pharmacokinetics of atorvastatin during simultaneous use
Drug used simultaneously and dosage regimen
Atorvastatin
Dose (mg)
Change
AUC
Clinical guidelines
Tipranavir 500 mg twice daily / Ritonavir 200 mg twice daily for 8 days (days 14-21)
40 mg per day 1
10 mg per day 20
9.4x magnification
In cases where the use of atorvastatin is necessary, the dose of atorvastatin should not exceed 10 mg per day. Patients require medical supervision.
Cyclosporine 5.2 mg/kg/day – constant dose
10 mg 1 time per day
8.7x magnification
Lopinavir 400 mg twice daily / Ritonavir twice daily for 14 days
20 mg once a day for 4 days
5.9x magnification
In cases where the use of atorvastatin is necessary, a reduction in the dose of atorvastatin is required. If the dose of atorvastatin exceeds 20 mg per day, medical supervision is required.
Clarithromycin 500 mg 2 times a day for 9 days
80 mg once daily for 8 days
4.4x magnification
Saquinavir 400 mg 2 times a day / Ritonavir 300 mg 2 times a day days 5-7, 400 mg from day 8, from 5 to 18 days – 30 minutes after taking atorvastatin
40 mg once daily for 4 days
3.9x magnification
In cases where the use of atorvastatin is necessary, a reduction in the dose of atorvastatin is required. If the dose of atorvastatin exceeds 40 mg per day, medical supervision is required.
Darunavir 300 mg twice daily / Ritonavir 100 mg twice daily for 9 days
10 mg once daily for 4 days
3.3x magnification
Itraconazole 200 mg once daily for 4 days
40 mg, single dose
3.3x magnification
Fozamprenavir 700 mg twice daily / Ritonavir 100 mg twice daily for 14 days
10 mg once daily for 4 days
2.5 times magnification
Fozamprenavir 1400 mg 2 times a day for 14 days
10 mg once daily for 4 days
2.3 times magnification
Nelfinavir 1250 mg 2 times a day for 14 days
10 mg once daily for 28 days
1.7x magnification
No dose adjustment required
Grapefruit juice, 240 ml once a day
40 mg, single dose
37% increase
Drinking significant amounts of grapefruit juice while taking atorvastatin is not recommended.
Diltiazem 240 mg once daily for 28 days
40 mg, single dose
51% increase
Medical supervision is required when prescribing or adjusting the dose of diltiazem.
Erythromycin 500 mg 4 times a day for 7 days
10 mg, single dose
33% increase
Adjustment of the maximum dose of atorvastatin is necessary and medical supervision is required
Amlodipine 10 mg, single dose
80 mg, single dose
18% increase
No dose adjustment required
Cimetidine 300 mg 4 times a day for 2 weeks
10 mg once daily for 4 weeks
Less than 1% reduction
No dose adjustment is required.
Suspension containing magnesium and aluminum 30 ml 4 times a day for 2 weeks
10 mg once daily for 4 weeks
35% reduction
No dose adjustment is required.
Efavirenz 600 mg once daily for 14 days
10 mg for 3 days
41% reduction
No dose adjustment is required.
Rifampicin 600 mg once a day for 7 days (simultaneous use)
40 mg, single dose
30% increase
If concomitant use with rifampicin cannot be avoided, medical supervision is required.
Rifampicin 600 mg once a day for 5 days (separate doses)
40 mg, single dose
80% reduction
Gemfibrozil 600 mg 2 times a day for 7 days
40 mg, single dose
35% increase
The initial dose should be reduced and medical supervision is required.
Fenofibrate 160 mg once daily for 7 days
40 mg, single dose
3% increase
The initial dose should be reduced and medical supervision is required.
Effect of atorvastatin on other drugs
Digoxin
With repeated administration of digoxin and atorvastatin at a dose of 10 mg, the equilibrium concentrations of digoxin in the blood plasma did not change. However, when digoxin was used in combination with atorvastatin at a dose of 80 mg/day, digoxin concentrations increased by approximately 20%.
Oral contraceptives
When atorvastatin was used concomitantly with an oral contraceptive containing norethisterone and ethinyl estradiol, an increase in plasma concentrations of norethisterone and ethinyl estradiol was observed. These increases in concentrations should be taken into account when choosing dosages of oral contraceptives. When atorvastatin was co-administered with an oral contraceptive containing norethisterone and ethinyl estradiol, a significant increase in the AUC of norethisterone and ethinyl estradiol by 30% and 20%, respectively, was observed. This effect should be taken into account when choosing an oral contraceptive for a woman receiving atorvastatin.
Warfarin
With simultaneous use of atorvastatin with warfarin, a slight decrease in prothrombin time was observed in the first days of taking atorvastatin; however, over the next 15 days, the prothrombin time returned to normal.
Table 2. Effects of atorvastatin on the pharmacokinetics of other drugs when used concomitantly.
Atorvastatin dosage regimen
Drug used at the same time
Drug/dose (mg)
Change in AUC
Clinical guidelines
80 mg once a day for 10 days
Digoxin 0.25 mg once a day for 20 days
15% increase
Medical supervision required
40 mg once daily for 22 days
Oral contraceptive once a day for 2 months
Norethindrone 1 mg
Ethinyl estradiol 35 mcg
Increase 28%
19% increase
No dose adjustment required
80 mg once daily for 15 days
Phenazone 600 mg, single dose
3% increase
No dose adjustment required
Overdose
Overdose
There is no specific antidote. In case of overdose, the necessary symptomatic and supportive therapy should be provided. Monitoring of liver function and serum CPK levels is necessary. Hemodialysis is ineffective.
Storage conditions
Storage conditions
Store at a temperature not exceeding 25 ºС.
Keep out of the reach of children!
Shelf life
Shelf life
2 years
Manufacturer
Manufacturer
Alkaloid AD Skopje, Republic of North Macedonia
Additional information
| Shelf life | 2 years |
|---|---|
| Conditions of storage | Store at a temperature not exceeding 25 ºC. Keep out of reach of children! |
| Manufacturer | Alkaloid AD Skopje, Republic of Northern Macedonia |
| Medication form | pills |
| Brand | Alkaloid AD Skopje |
Other forms…
Related products
Buy Atorvastatin-Teva, 20 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.