No products in the cart.
Atorvastatin-SZ, 10 mg 30 pcs
€3.76 €3.35
Description
Cholesterol, Atherosclerosis, Cholesterol Reduction, Prevention of heart attacks and strokes
– Primary hypercholesterolemia (heterozygous familial and non-family hypercholesterolemia (type IIa according to Fredrickson classification);
– Combined (mixed) hyperlipidemia (Fredrickson classification types IIa and IIb);
– Dysbetalipoproteinemia (Fredrickson classification type III) (as an adjunct to diet);
– Familial endogenous hypertriglyceridemia (Fredrickson classification type IV), resistant to diet;
– Homozygous familial hypercholesterolemia when diet therapy and other non-pharmacological treatments are not effective;
– Prevention of cardiovascular disease:
– Primary prevention of cardiovascular complications in patients without clinical signs of coronary heart disease (CHD) but who have several risk factors for its development: age over 55 years, nicotine addiction, arterial hypertension, diabetes mellitus, genetic predisposition, including on the background of dyslipidemia;
– Secondary prevention of cardiovascular complications in patients with CHD to reduce the total mortality rate, myocardial infarction, stroke, repeated hospitalization for angina and the need for revascularization.
Indications
Indications
• Primary hypercholesterolemia (heterozygous familial and non-familial hypercholesterolemia (type IIa according to the Fredrickson classification);
• Combined (mixed) hyperlipidemia (types IIa and IIb according to the Fredrickson classification);
• Disbetalipoproteinemia (type III according to the Fredrickson classification) (as an addition to the diet);
• Familial endogenous hypertriglyceridemia (type IV according to the Fredrickson classification), resistant to diet;
• Homozygous familial hypercholesterolemia with insufficient effectiveness of diet therapy and other non-pharmacological treatment methods;
• Prevention of cardiovascular diseases:
– Primary prevention of cardiovascular complications in patients without clinical signs of coronary heart disease (CHD), but with several risk factors for its development: age over 55 years, nicotine addiction, hypertension, diabetes mellitus, genetic predisposition, including dyslipidemia;
– Secondary prevention of cardiovascular complications in patients with coronary artery disease in order to reduce the total mortality rate, myocardial infarction, stroke, re-hospitalization for angina pectoris and the need for revascularization.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group of the drug:
Special instructions
Special instructions
Before starting Atorvastatin therapy, the patient must be prescribed a standard cholesterol-lowering diet, which he must follow during the entire treatment period. The use of HMG-CoA reductase inhibitors to reduce blood lipid levels can lead to changes in biochemical parameters reflecting liver function.
Liver function should be monitored before starting therapy, 6 weeks, 12 weeks after starting Atorvastatin and after each dose increase, and periodically, for example, every 6 months. An increase in the activity of liver enzymes in the blood serum may be observed during therapy with Atorvastatin. Patients who experience elevated enzyme levels should be monitored until enzyme levels return to normal.
If alanine aminotransferase (ALT) or aspartic aminotransferase (AST) values are more than 3 times the upper acceptable limit, it is recommended to reduce the dose of Atorvastatin or discontinue treatment. Atorvastatin should be used with caution in patients who abuse alcohol and/or have liver disease.
Active liver disease or persistent increases in aminotransferase activity of unknown origin are contraindications to the use of Atorvastatin. Treatment with Atorvastatin may cause myopathy. The diagnosis of myopathy (muscle pain and weakness in combination with an increase in creatine phosphokinase (CPK) activity more than 10 times the upper limit of normal) should be considered in patients with widespread myalgia, muscle soreness or weakness, and/or a marked increase in CPK activity. Patients should be warned that they should immediately tell their doctor if they experience unexplained muscle pain or weakness if they are accompanied by malaise or fever.
Atorvastatin therapy should be discontinued in the event of a marked increase in CPK activity or in the presence of confirmed or suspected myopathy. The risk of myopathy during treatment with other drugs in this class was increased with concomitant use of cyclosporine, fibrates, erythromycin, niacin, or azole antifungals. Many of these drugs inhibit cytochrome P450 3A4-mediated metabolism and/or drug transport.
Atorvastatin is biotransformed by CYP 3A4. When prescribing Atorvastatin in combination with fibrates, erythromycin, immunosuppressive agents, azole antifungals or nicotinic acid in lipid-lowering doses, the expected benefits and risks of treatment should be carefully weighed and patients should be regularly monitored for muscle pain or weakness, especially during the first months of treatment and during periods of increasing dosage of any drug. In such situations, periodic determination of CPK activity can be recommended, although such monitoring does not prevent the development of severe myopathy.
When using Atorvastatin, as well as other drugs of this class, cases of rhabdomyolysis with acute renal failure caused by myoglobinuria have been described. Atorvastatin therapy should be temporarily discontinued or completely discontinued if signs of possible myopathy appear or if there is a risk factor for the development of renal failure due to rhabdomyolysis (for example, severe acute infection, hypotension, major surgery, trauma, severe metabolic, endocrine and electrolyte disturbances, and uncontrolled seizures).
Before starting therapy with Atorvastatin, an attempt should be made to control hypercholesterolemia through adequate diet therapy, increased physical activity, weight loss in obese patients, and treatment of other conditions. Patients should be warned to seek immediate medical attention if they experience unexplained muscle pain or weakness, especially if accompanied by malaise or fever.
Active ingredient
Active ingredient
Atorvastatin
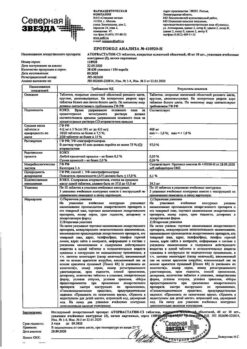
Composition
Composition
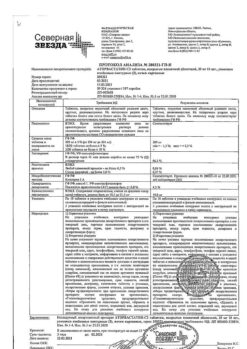
dosage 10 mg of active substance:
atorvastatin calcium in terms of atorvastatin – 10 mg
excipients (core):
lactose monohydrate (milk sugar) – 62.0 mg; calcium carbonate – 33.0 mg; povidone K 30 (medium molecular weight polyvinylpyrrolidone) – 6.0 mg; croscarmellose sodium (primellose) – 6.75 mg; sodium stearyl fumarate – 1.5 mg; colloidal silicon dioxide (Aerosil) – 0.75 mg; microcrystalline cellulose – 30.0 mg;
excipients (shell):
Opadry II (polyvinyl alcohol, partially hydrolyzed – 2.2 mg; macrogol (polyethylene glycol) 3350 – 0.6175 mg; talc – 1.0 mg; titanium dioxide E 171 – 0.9585 mg; soy lecithin E 322 – 0.175 mg; aluminum varnish based on indigo carmine dye – 0.003 mg; aluminum varnish based on azorubine dye – 0.0255 mg; aluminum varnish based on crimson dye [Ponceau 4R] – 0.0205 mg).
Tablets, film-coated, pink, round, biconvex.
In cross-section, the core of the tablet is white or almost white.
Contraindications
Contraindications
Hypersensitivity to any component of the drug. Active liver disease or an increase in the activity of “liver” transaminases in the blood plasma of unknown origin by more than 3 times compared with the upper limit of normal. Age under 18 years (insufficient clinical data on the effectiveness and safety of the drug in this age group). Lactose intolerance, lactase deficiency, glucose-galactose malabsorption. Hypersensitivity to soy and peanuts. Pregnancy and breastfeeding period. Use in women planning pregnancy and not using reliable methods of contraception.
With caution
Alcohol abuse, history of liver disease, diseases of the muscular system (history of the use of other representatives of the group of HMG-CoA reductase inhibitors), severe disturbances of water and electrolyte balance, endocrine (hyperthyroidism) and metabolic disorders, severe acute infections (sepsis), arterial hypotension, diabetes mellitus, uncontrolled epilepsy, extensive surgical interventions, trauma.
Side Effects
Side Effects
In controlled clinical trials (n=2502), less than 2% of patients discontinued treatment due to side effects caused by atorvastatin.
The most common adverse effects associated with atorvastatin were constipation, flatulence, dyspepsia and abdominal pain.
From the nervous system and sensory organs: ≥2% – headache, asthenic syndrome, insomnia, dizziness;
From the cardiovascular system: ≥2% – chest pain; blood pressure, phlebitis, arrhythmia, angina pectoris, anemia, lymphadenopathy, thrombocytopenia.
From the respiratory system: ≥2% – sinusitis, pharyngitis, bronchitis, rhinitis;
From the gastrointestinal tract: ≥2% – abdominal pain, constipation or diarrhea, dyspepsia, flatulence, nausea;
From the musculoskeletal system: ≥2% – arthralgia, myalgia, arthritis;
From the genitourinary system: ≥2% – urogenital infections, peripheral edema;
From the skin:
Allergic reactions: ≥2% – skin rash;
Other: ≥2% – infections, accidental trauma, influenza-like syndrome, back pain; ALP, increased ALT or AST, exacerbation of gout.
Side effects noted in post-marketing studies with atorvastatin therapy: anaphylaxis, angioedema, bullous rash (including erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis), rhabdomyolysis, tendon rupture.
Interaction
Interaction
The risk of myopathy during treatment with HMG-CoA reductase inhibitors increases with simultaneous use of cyclosporine, fibrates, antibiotics (erythromycin, clarithromycin, quinupristin/dalfopristin), nefazodone, HIV protease inhibitors (indinavir, ritonavir), colchicine, azole derivative antifungals, and nicotinic acid in lipid-lowering doses (more than 1 g/day) (see section “Special instructions”).
CYP3A4 isoenzyme inhibitors
Since atorvastatin is metabolized by the CYP3A4 isoenzyme, the combined use of atorvastatin with inhibitors of the CYP3A4 isoenzyme may lead to an increase in the concentration of atorvastatin in the blood plasma. The degree of interaction and potentiation effect are determined by the variability of the effect on the CYP3A4 isoenzyme.
Inhibitors of the transport protein OATP1B1
Atorvastatin and its metabolites are substrates of the transport protein OATP1B1. OATP1B1 inhibitors (eg, cyclosporine) may increase the bioavailability of atorvastatin. Thus, the combined use of atorvastatin at a dose of 10 mg and cyclosporine at a dose of 5.2 mg/kg/day leads to an increase in the concentration of atorvastatin in the blood plasma by 7.7 times. If simultaneous use with cyclosporine is necessary, the dose of Atorvastatin-SZ should not exceed 10 mg/day (see section “Dosage and Administration”).
Erythromycin/clarithromycin
With the simultaneous use of atorvastatin and erythromycin (500 mg 4 times a day) or clarithromycin (500 mg 2 times a day), which inhibit the CYP3A4 isoenzyme, an increase in the concentration of atorvastatin in the blood plasma was observed (see section “Special instructions”). Caution should be used to use the lowest effective dose of atorvastatin when coadministered with clarithromycin.
Protease inhibitors
The simultaneous use of atorvastatin with protease inhibitors, known as CYP3A4 isoenzyme inhibitors, is accompanied by an increase in the concentration of atorvastatin in the blood plasma (when used simultaneously with erythromycin, the Cmax of atorvastatin increases by 40%).
Combination of protease inhibitors
Patients taking HIV protease inhibitors and hepatitis C inhibitors should use caution and use the lowest effective dose of atorvastatin. In patients taking telaprevir or the tipranavir/ritonavir combination, the dose of Atorvastatin-SZ should not exceed 10 mg/day.
Patients taking the HIV protease inhibitor tipranavir plus ritonavir or the hepatitis C protease inhibitor telaprevir should avoid concomitant use of Atorvastatin-SZ. For patients taking the HIV protease inhibitors lopinavir plus ritonavir, caution should be exercised when prescribing Atorvastatin-SZ and the lowest dose required should be prescribed. In patients taking the HIV protease inhibitors saquinavir plus ritonavir, darunavir plus ritonavir, fosamprenavir, or fosamprenavir plus ritonavir, the dose of Atorvastatin-SZ should not exceed 20 mg and the drug should be used with caution. In patients taking the HIV protease inhibitor nelfinavir or the hepatitis C protease inhibitor boceprevir, the dose of Atorvastatin-SZ should not exceed 40 mg and close clinical monitoring is recommended.
Diltiazem
The combined use of atorvastatin at a dose of 40 mg with diltiazem at a dose of 240 mg leads to an increase in the concentration of atorvastatin in the blood plasma.
Ketoconazole, spironolactone and cimetidine
Caution should be exercised when atorvastatin is used concomitantly with drugs that reduce the concentration of endogenous steroid hormones, such as ketoconazole, spironolactone and cimetidine.
Itraconazole
Concomitant use of atorvastatin in doses from 20 mg to 40 mg and itraconazole in a dose of 200 mg led to an increase in the AUC value of atorvastatin. Caution should be used to use the lowest effective dose of atorvastatin when coadministered with itraconazole.
Grapefruit juice
Since grapefruit juice contains one or more components that inhibit the CYP3A4 isoenzyme, excessive consumption (more than 1.2 L per day) may cause an increase in plasma concentrations of atorvastatin.
Inducers of the CYP3A4 isoenzyme
The combined use of atorvastatin with inducers of the CYP3A4 isoenzyme (for example, efavirenz, phenytoin or rifampicin) may lead to a decrease in the concentration of atorvastatin in the blood plasma. Due to the dual mechanism of interaction with rifampicin (an inducer of the CYP3A4 isoenzyme and an inhibitor of the hepatocyte transport protein OATP1B1), simultaneous use of atorvastatin and rifampicin is recommended, since delayed administration of atorvastatin after taking rifampicin leads to a significant decrease in the concentration of atorvastatin in the blood plasma.
Antacids
Simultaneous oral administration of a suspension containing magnesium hydroxide and aluminum hydroxide reduced the concentration of atorvastatin in the blood plasma by approximately 35%, but the degree of reduction in the concentration of LDL-C did not change.
Phenazone
Atorvastatin does not affect the pharmacokinetics of phenazone, so interaction with other drugs metabolized by the same cytochrome isoenzymes is not expected.
Colestipol
With simultaneous use of colestipol, the concentration of atorvastatin in the blood plasma decreased by approximately 25%; however, the lipid-lowering effect of the combination of atorvastatin and colestipol was superior to that of each drug alone.
Digoxin
With repeated administration of digoxin and atorvastatin at a dose of 10 mg, the equilibrium concentrations of digoxin in the blood plasma did not change. However, when using digoxin in combination with atorvastatin at a dose of 80 mg/day. digoxin concentration increased by approximately 20%.
Patients receiving digoxin in combination with atorvastatin require appropriate monitoring.
Azithromycin
With simultaneous use of atorvastatin at a dose of 10 mg 1 time per day and azithromycin at a dose of 500 mg 1 time per day, the concentration of atorvastatin in the blood plasma did not change.
Oral contraceptives
When atorvastatin was coadministered with an oral contraceptive containing norethisterone and ethinyl estradiol, significant increases in the AUC of norethisterone and ethinyl estradiol by approximately 30% and 20%, respectively, were observed. This effect should be taken into account when choosing an oral contraceptive for a woman taking atorvastatin.
Terfenadine
With simultaneous use of atorvastatin and terfenadine, no clinically significant changes in the pharmacokinetics of terfenadine were detected.
Warfarin
Concomitant use of atorvastatin with warfarin may increase the effect of warfarin on blood coagulation parameters (decreased prothrombin time) in the first days. This effect disappears after 15 days of simultaneous use of these drugs.
Amlodipine
With simultaneous use of atorvastatin at a dose of 80 mg and amlodipine at a dose of 10 mg, the pharmacokinetics of atorvastatin at steady state did not change.
Other concomitant therapy
In clinical studies, atorvastatin was used in combination with antihypertensive agents and estrogens as part of replacement therapy; there were no signs of clinically significant adverse interactions; No interaction studies with specific drugs have been conducted.
Overdose
Overdose
In case of overdose, the following general measures are necessary: monitoring and maintaining vital functions of the body, as well as preventing further absorption of the drug (gastric lavage, taking activated charcoal or laxatives).
Storage conditions
Storage conditions
Store in a dry place, protected from light, out of reach of children, at a temperature of 15 C to 30 C.
Shelf life
Shelf life
2 years.
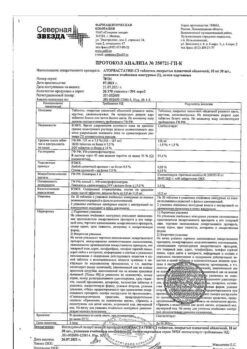
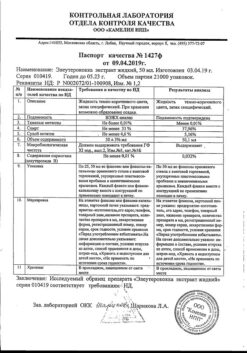
Manufacturer
Manufacturer
North Star NAO, Russia
Additional information
| Shelf life | 2 years. |
|---|---|
| Conditions of storage | Store in a dry place protected from light, out of the reach of children, at a temperature of 15 C to 30 C. |
| Manufacturer | North Star NAO, Russia |
| Medication form | pills |
| Brand | North Star NAO |
Other forms…
Related products
Buy Atorvastatin-SZ, 10 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.