No products in the cart.
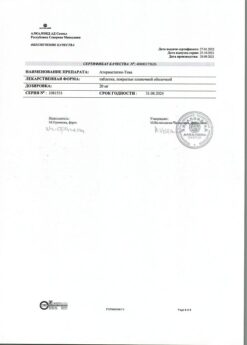
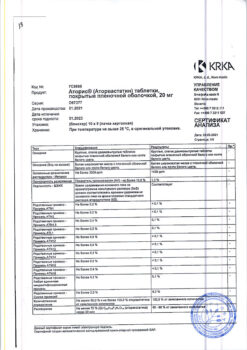
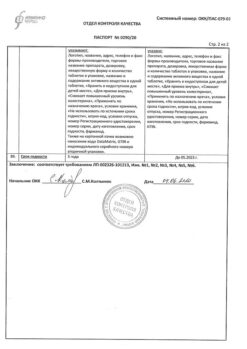
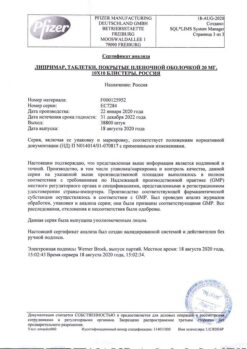
Atorvastatin, 40 mg 30 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
Atorvastatin is a hypolipidemic drug from the group of statins.
By the principle of competitive antagonism the statin molecule binds to the part of the coenzyme A receptor where HMG-CoA reductase is attached. The other part of the statin molecule inhibits the conversion of hydroxymethylglutarate into mevalonate, an intermediate product in the synthesis of the cholesterol molecule.
Inhibition of HMG-CoA reductase activity leads to a series of sequential reactions resulting in a decrease in intracellular cholesterol content and a compensatory increase in LDL-receptor activity and corresponding acceleration of LDL cholesterol (Xc) catabolism.
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
Active ingredient:
atorvastatin calcium trihydrate;
Associates:
calcium carbonate;
MCC;
StarCap1500 (corn starch and pregelatinized starch);
silica colloidal dioxide (aerosil);
p> talc;
magnesium stearate;
Opadry II (series 85) (polyvinyl alcohol, macrogol, talc, titanium dioxide, iron oxide yellow dye, iron oxide red dye).
How to take, the dosage
How to take, the dosage
Ingestion.
Before prescribing Atorvastatin, a standard hypolipidemic diet should be recommended for the patient, which the patient should continue to follow during the entire period of therapy.
The initial dose is on average 10 mg/day. The dose varies from 10 to 80 mg/day.
The drug can be taken at any time of the day with food or regardless of the time of meals. The dose is adjusted with regard to baseline cholesterol/LDL levels, the goal of therapy, and individual effect. At the beginning of treatment and/or during dose increase of Atorvastatin it is necessary to monitor plasma lipid levels every 2-4 weeks and adjust the dose accordingly.
In order to ensure the following dosing regimen of the drug it is possible to use Atorvastatin in other dosage forms: film-coated tablets 10 mg and 20 mg. The maximum daily dose of the drug is 80 mg.
In concomitant use with cyclosporine, the daily dose of Atorvastatin should not exceed 10 mg.
Primary hypercholesterolemia and mixed hyperlipidemia. In most cases, it is sufficient to prescribe a dose of 10 mg of Atorvastatin once daily. Significant therapeutic effect is observed after 2 weeks, and the maximum therapeutic effect is usually observed after 4 weeks. With long-term treatment this effect is maintained.
Patient special groups
Kidney function disorders. Administration of the drug in patients with renal insufficiency and renal diseases does not influence on plasma levels of Atorvastatin or degree of cholesterol/LDL decrease with its use, therefore no change of drug dose is required.
Hepatic disorders. In case of hepatic insufficiency, the dose should be reduced.
Elderly patients. No differences in safety, efficacy or achievement of hypolipidemic therapy goals have been noted when using the drug in elderly patients compared to the general population.
Interaction
Interaction
The risk of myopathy during treatment with other statin-derived drugs is increased with concomitant use of cyclosporine, fibrates, erythromycin, azole antifungals and nicotinic acid. When concomitant administration of Atorvastatin and suspension containing magnesium hydroxide and aluminum hydroxide, plasma concentration of Atorvastatin was decreased by approximately 35%, but the degree of decrease in HDL-C levels did not change.
In concomitant use Atorvastatin does not affect pharmacokinetics of antipyrine (phenazone), therefore interaction with other drugs metabolized by the same cytochrome P450 isoenzymes is not expected.
Special Instructions
Special Instructions
Before starting therapy with Atorvastatin, a standard hypocholesterolemic diet should be prescribed to the patient, which should be followed during the entire period of treatment. The use of HMG-CoA reductase inhibitors to reduce blood lipid levels may lead to changes in biochemical parameters reflecting liver function. Liver function should be monitored before the start of therapy, at 6 weeks, 12 weeks after the start of Atorvastatin and after each dose increase as well as periodically, e.g., every 6 months.
Elevated serum hepatic enzyme activity may be observed during therapy with Atorvastatin. Patients with increased enzyme levels should be monitored until enzyme levels return to normal. If alanine aminotransferase (ALT) or asparagine aminotransferase (AST) values are more than 3 times higher than the upper allowable limit, it is recommended to reduce the dose of Atorvastatin or discontinue treatment. Atorvastatin should be used with caution in patients who abuse alcohol and/or have liver disease. Active liver disease or persistent increase in aminotransferase activity of unclear genesis are contraindications to Atorvastatin administration.
Treatment with Atorvastatin may cause myopathy. The diagnosis of myopathy (pain and weakness in muscles combined with an increase in creatine phosphokinase (CPK) activity more than 10 times the upper limit of normal) should be discussed in patients with widespread myalgia, muscle soreness or weakness and/or marked increase in CPK activity. Patients should be warned to inform their physician immediately of unexplained muscle pain or weakness if accompanied by malaise or fever. Atorvastatin therapy should be discontinued in case of marked increase in CPK activity or in the presence of confirmed or suspected myopathy. Risk of myopathy during treatment with other drugs of this class was increased with concomitant use of cyclosporine, fibrates, erythromycin, nicotinic acid or azole antifungal agents.
Many of these drugs inhibit cytochrome P450 3A4-mediated metabolism and/or drug transport. Atorvastatin is biotransformed by CYP 3A4. Prescribing Atorvastatin in combination with fibrates, erythromycin, immunosuppressive agents, azole antifungal agents or nicotinic acid in hypolipidemic doses, the expected benefits and risks of treatment should be carefully weighed and patients should be regularly observed to detect muscle pain or weakness, especially during the first months of treatment and during periods of increasing doses of any drug. In such situations, periodic determination of CPK activity may be recommended, although such monitoring does not prevent the development of severe myopathy.
In Atorvastatin, as well as other drugs of this class, there have been cases of rhabdomyolysis with acute renal failure due to myoglobinuria. Atorvastatin therapy should be temporarily discontinued or completely discontinued in case of signs of possible myopathy or in presence of risk factor of renal failure during rhabdomyolysis (for example, severe acute infection, arterial hypotension, serious surgery, trauma, severe metabolic, endocrine and electrolyte disorders and uncontrolled convulsions).
Before starting therapy with Atorvastatin, an attempt should be made to achieve control of hypercholesterolemia through adequate diet therapy, increasing physical activity, reducing body weight in obese patients and treating other conditions. Patients should be warned to seek immediate medical attention if they experience unexplained muscle pain or weakness, especially if accompanied by malaise or fever.
Contraindications
Contraindications
Side effects
Side effects
Nervous system disorders: insomnia, dizziness; headache, asthenia, malaise, somnolence, nightmares, paresthesias, peripheral neuropathy, amnesia, emotional lability, ataxia, facial nerve paralysis, hyperkinesias, migraine, depression, hypoesthesia, loss of consciousness.
Senses: amblyopia, tinnitus, dry conjunctiva, accommodation disorder, retinal hemorrhage, deafness, glaucoma, parosmia, loss of sense of taste, perversion of taste.
Cardiovascular system: chest pain; palpitations, symptoms of vasodilation, orthostatic hypotension, increased BP, phlebitis, arrhythmias, angina pectoris.
Hematopoietic system disorders: anemia, lymphoadenopathy, thrombocytopenia.
Respiratory system: bronchitis, rhinitis; pneumonia, dyspnea, exacerbation of bronchial asthma, nasal bleeding.
Digestive system disorders: nausea; heartburn, constipation or diarrhea, flatulence, gastralgia, abdominal pain, decreased or increased appetite, dry mouth, belching, dysphagia, vomiting, stomatitis, esophagitis, glossitis, erosive and ulcerative lesions of the oral mucosa, gastroenteritis, hepatitis, biliary colic, cheilitis, duodenal ulcer, pancreatitis, cholestatic jaundice, liver dysfunction, rectal bleeding, melena, bleeding gums, tenesmus.
Muscular system disorders: arthritis; leg muscle cramps, bursitis, tenosynovitis, myositis, myopathy, arthralgia, myalgia, rhabdomyolysis, torticollis, muscle hypertonicity, joint contractures, joint swelling, tendopathy (in some cases with tendon rupture).
Urogenital system: urogenital infections, peripheral edema; < 1% – dysuria (including Pollakiuria, nycturia, urinary incontinence or urinary retention, imperative urge to urinate), leukocyturia, nephritis, hematuria, vaginal bleeding, nephrourolithiasis, metrorrhagia, epididymitis, decreased libido, impotence, ejaculation disorders.
Dermatological reactions: alopecia, xeroderma, photosensitization, increased sweating, eczema, seborrhea, ecchymoses, petechiae.
Endocrine system disorders: gynecomastia, mastodynia.
Metabolism disorders: weight gain, aggravation of gout.
Allergic reactions: skin itching, skin rash, contact dermatitis, rarely – urticaria, angioedema, facial edema, anaphylaxis, erythema multiforme (including Stevens-Johnson syndrome), toxic epidermal necrolysis (Lyell’s syndrome).
Laboratory measures: hyperglycemia, hypoglycemia, increased serum CPK, albuminuria.
Overdose
Overdose
Treatment: there is no specific antidote, symptomatic therapy is carried out. Hemodialysis is ineffective.
Similarities
Similarities
Additional information
| Shelf life | 2 years. |
|---|---|
| Conditions of storage | Store in a dry place protected from light, out of the reach of children, at a temperature of 15 C to 30 C. |
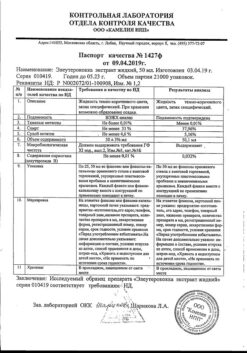
| Manufacturer | Kanonfarma Production ZAO, Russia |
| Medication form | pills |
| Brand | Kanonfarma Production ZAO |
Other forms…
Related products
Buy Atorvastatin, 40 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.