No products in the cart.
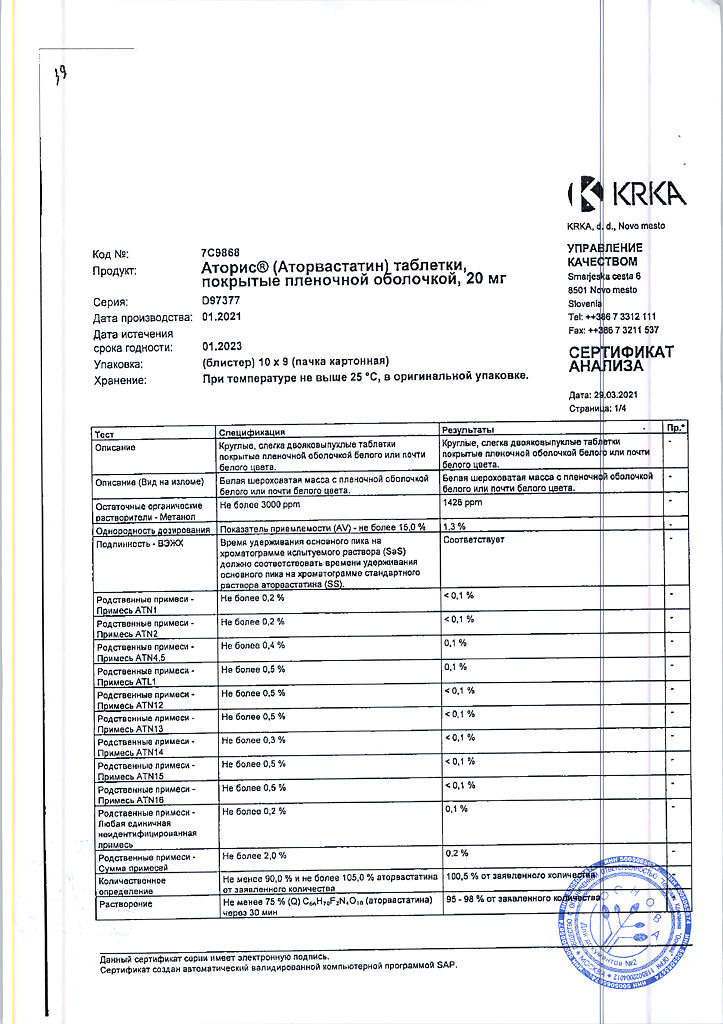
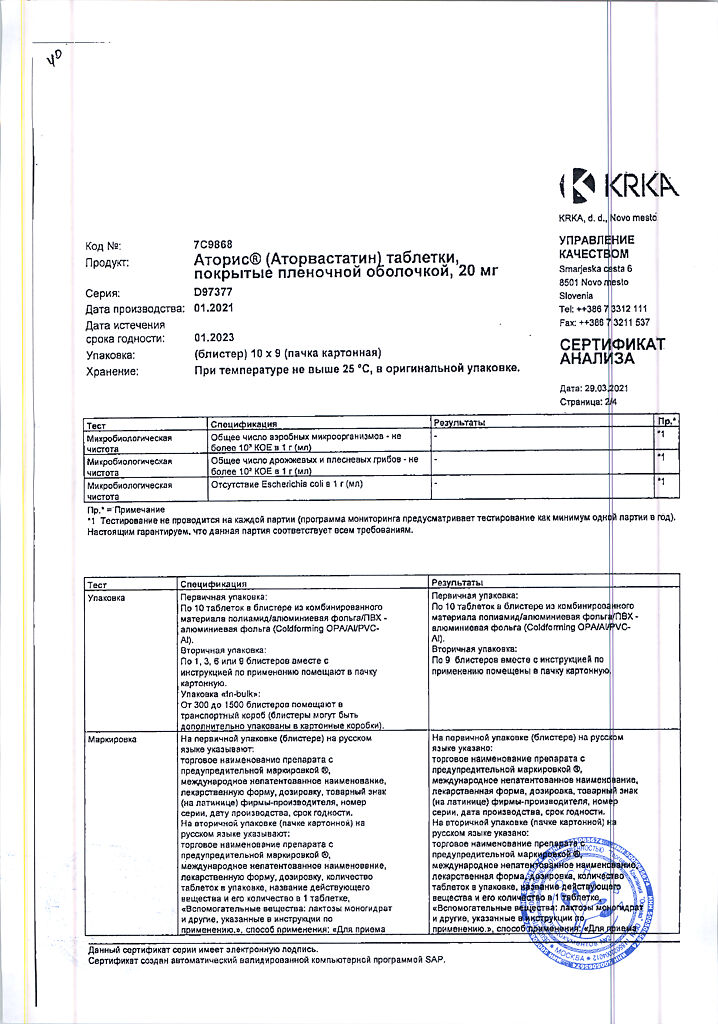
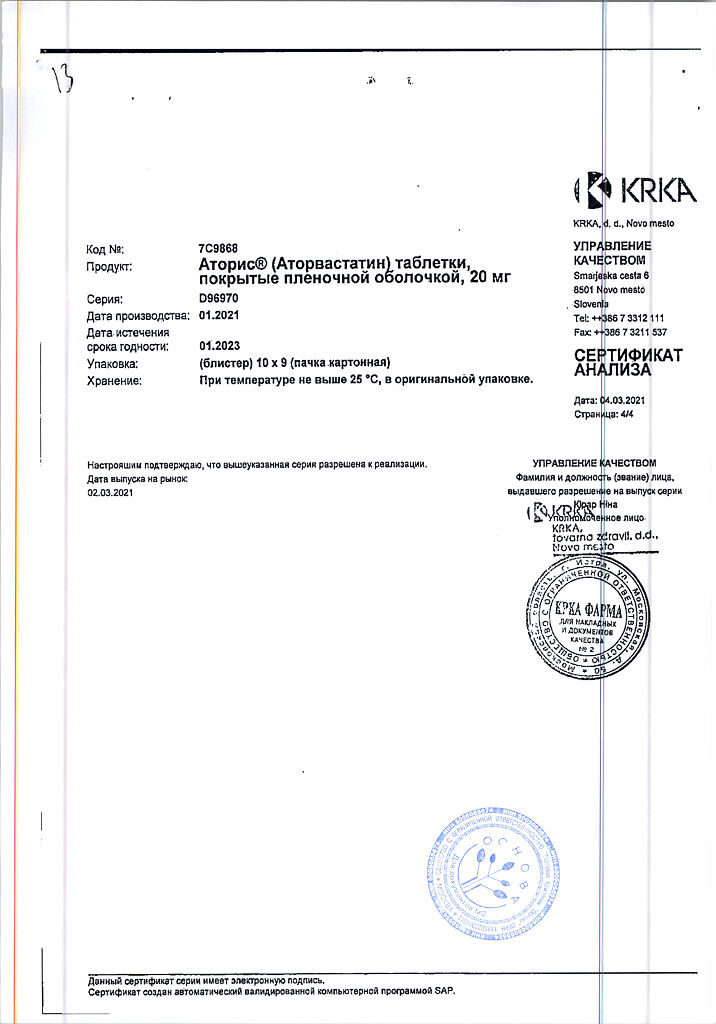
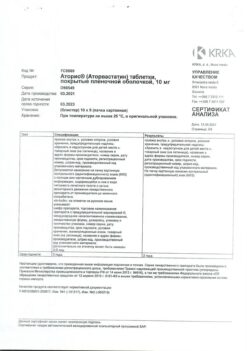
Atoris, 20 mg 90 pcs.
€30.01 €25.01
Description
Cholesterol, Heart attack and stroke prevention, Cholesterol reduction
Hypercholesterolemia:
– to reduce elevated total CH, LDL-C in adults with homozygous familial hypercholesterolemia as a supplement to other hypolipidemic therapies (such as LDL–apheresis), or if such treatments are not available.
– Prevent cardiovascular disease:
– prevention of cardiovascular events in adult patients at high risk of developing primary cardiovascular events, as an adjunct to correction of other risk factors;
– secondary prevention of cardiac–-vascular complications in patients with CHD to reduce mortality, MI, strokes, repeat hospitalizations for angina and need for revascularization.
Indications
Indications
Hypercholesterolemia:
– as an adjunct to diet to reduce elevated total cholesterol, LDL-C, apo-B and TG in adults, adolescents and children 10 years of age or older with primary hypercholesterolemia, including familial hypercholesterolemia (heterozygous variant) or combined (mixed variant) hyperlipidemia (Fredrickson type IIa and IIb, respectively), when responsive to diet and other non-drug treatments insufficient;
– to reduce elevated total cholesterol and LDL cholesterol in adults with homozygous familial hypercholesterolemia as an adjunct to other lipid-lowering treatments (eg, LDL apheresis), or if such treatments are not available.
· Prevention of cardiovascular diseases:
– prevention of cardiovascular events in adult patients at high risk of developing primary cardiovascular events, as an addition to the correction of other risk factors;
– secondary prevention of cardiovascular complications in patients with coronary artery disease in order to reduce mortality, MI, strokes, re-hospitalization for angina pectoris and the need for revascularization.
Pharmacological effect
Pharmacological effect
lipid-lowering agent – HMG-CoA reductase inhibitor
Special instructions
Special instructions
In patients with risk factors for the development of rhabdomyolysis (impaired renal function, hypothyroidism, a patient’s history or family history of hereditary muscle disorders, previous toxic effects of HMG-CoA reductase inhibitors [statins] or fibrates on muscle tissue, a history of liver disease and/or patients who drink significant amounts of alcohol, age over 70 years, situations in which increased concentrations of atorvastatin are expected in patients blood plasma [for example, interactions with other drugs]).
Contraindicated in persons under 18 years of age (there is insufficient clinical data on the effectiveness and safety of the drug in this age group), with the exception of heterozygous familial hypercholesterolemia (use is contraindicated in children under 10 years of age).
Children aged 10 to 17 years treated with atorvastatin had an adverse event profile similar to that of placebo-treated patients, with infections being the most common adverse event in both groups, regardless of assessment of causality. In the 3-year study, there were no clinically significant effects on growth and puberty as measured by the Global Maturation and Development Assessment, Tanner Stage Assessment, and Height and Weight Measurements. The safety and tolerability profile in children was similar to the known safety profile of atorvastatin in adults.
The clinical safety database includes safety data for 520 children treated with atorvastatin, of which 7 patients were aged <6 years, 121 patients were aged 6 to 9 years, and 392 patients were aged 10 to 17 years. Based on available data, the incidence, type and severity of adverse reactions in children are similar to those in adults.
In an 8-week open-label study, children with a Tanner score of 1 (N = 15) and ≥ 2 (N = 24) (aged 6–17 years) with heterozygous familial hypercholesterolemia and a baseline LDL-C concentration ≥ 4 mmol/L received atorvastatin therapy as 5 mg or 10 mg chewable tablets or film-coated tablets. shell, at a dose of 10 mg or 20 mg 1 time per day, respectively. The only significant covariate in the pharmacokinetic model of the atorvastatin population was body weight. The apparent clearance of atorvastatin in children did not differ from that in adult patients when allometrically measured by body weight. In the range of action of atorvastatin and o-hydroxyatorvastatin, there was a consistent decrease in LDL-C and cholesterol
Renal dysfunction
Impaired renal function does not affect the concentration of atorvastatin in the blood plasma or lipid metabolism, and therefore no dose adjustment is required in patients with impaired renal function.
There have been no studies of atorvastatin in patients with end-stage renal disease. Atorvastatin is not excreted during hemodialysis due to intense binding to plasma proteins.
Liver dysfunction
The concentration of the drug is significantly increased (Cmax – approximately 16 times, AUC – approximately 11 times) in patients with alcoholic cirrhosis of the liver (class B according to the Child-Pugh classification).
Hepatic uptake of all HMG-CoA reductase inhibitors, including atorvastatin, occurs with the participation of the OATP1B1 transporter. Patients with the SLCO1B1 genetic polymorphism are at risk of increased atorvastatin exposure, which may lead to an increased risk of rhabdomyolysis. The polymorphism of the gene encoding OATP1B1 (SLCO1B1 c.521CC) is associated with an increase in atorvastatin exposure (AUC) by 2.4 times compared to patients without such a genotypic change (c.521TT). These patients may also have impaired hepatic uptake of atorvastatin due to genetic disorders. Potential effects on effectiveness are unknown.
Elderly patients
Plasma concentrations of atorvastatin in patients over 65 years of age are higher (Cmax – approximately 40%, AUC – approximately 30%) than in young adult patients. There were no differences in the effectiveness and safety of the drug, as well as in achieving the goals of lipid-lowering therapy in elderly patients compared with the general population.
Effect on the liver
As with the use of other lipid-lowering drugs of this class, when using atorvastatin, a moderate increase (more than 3 times compared with the upper limit of normal) in the activity of hepatic transaminases AST and ALT in the blood plasma was noted. A persistent increase in serum activity of hepatic transaminases (more than 3 times the upper limit of normal) was observed in 0.7% of patients receiving atorvastatin. The incidence of such changes when using atorvastatin at doses of 10 mg, 20 mg, 40 mg and 80 mg was 0.2%, 0.2%, 0.6% and 2.3%, respectively. An increase in the activity of “liver” transaminases in the blood plasma was usually not accompanied by jaundice or other clinical manifestations. When the dose of atorvastatin was reduced, or the drug was temporarily or completely discontinued, the activity of “liver” transaminases in the blood plasma returned to the initial level. Most patients continued to take atorvastatin at a reduced dose without any clinical consequences.
Before starting therapy, 6 weeks and 12 weeks after starting the use of Atoris®, or after increasing its dose, it is necessary to monitor liver function indicators. Liver function should also be monitored when clinical signs of liver damage appear. In case of increased activity of “liver” transaminases in the blood plasma, the activity of ALT and AST in the blood plasma should be monitored until it returns to normal. If an increase in the activity of AST or ALT in the blood plasma by more than 3 times compared to the upper limit of normal persists, it is recommended to reduce the dose or discontinue the drug Atoris® (see section “Side effects”).
Atoris® should be used with caution in patients who drink significant amounts of alcohol and/or have a history of liver disease. Active liver disease or persistently increased activity of hepatic transaminases of unknown origin are a contraindication to the use of the drug Atoris® (see section “Contraindications”).
Action on skeletal muscles
Myalgia was observed in patients receiving atorvastatin (see section “Side effects”). The diagnosis of myopathy should be considered in patients with diffuse myalgia, muscle soreness or weakness, and/or a marked increase in serum CPK activity (more than 10 times the upper limit of normal). Therapy with Atoris® should be discontinued in the event of a marked increase in serum CPK activity, in the presence of confirmed myopathy or suspicion of its development. The risk of developing myopathy increases with the simultaneous use of drugs that increase the concentration of atorvastatin in the blood plasma (see sections “Interaction with other drugs” and “Pharmacological properties. Pharmacokinetics”), such as potent inhibitors of the CYP3A4 isoenzyme or carrier proteins (for example, cyclosporine, telithromycin, clarithromycin, delavirdine, stiripentol, ketoconazole, voriconazole, itraconazole, posaconazole and HIV protease inhibitors, including ritonavir, lopinavir, atazanavir, indinavir, darunavir, tipranavir/ritonavir, etc.), gemfibrozil or other fibrates, antiviral drugs for the treatment of HCV (boceprevir, telaprevir, elbasvir/grazoprevir), erythromycin, nicotinic acid in lipid-lowering doses (more than 1 g/day), ezetimibe, azole antifungals, colchicine. Many of these drugs inhibit CYP3A4-mediated metabolism and/or drug transport. It is known that the CYP3A4 isoenzyme is the main liver isoenzyme involved in the biotransformation of atorvastatin. When using the drug Atoris® in combination with fibrates, erythromycin, immunosuppressants, azole antifungals or nicotinic acid in lipid-lowering doses (more than 1 g / day), the doctor must carefully weigh the expected benefits of treatment and the possible risks. Patients should be regularly monitored for muscle pain or weakness, especially during the first months of therapy and during dosage increases of any of these agents. If combination therapy is necessary, the use of lower initial and maintenance doses of the above drugs should be considered (see section “Dosage and Administration”). The simultaneous use of atorvastatin and fusidic acid is not recommended, therefore, temporary withdrawal of atorvastatin is recommended during treatment with fusidic acid. In such situations, periodic monitoring of serum CPK activity can be recommended, although such monitoring does not prevent the development of severe myopathy (see section “Interaction with other drugs”).
Before treatment
Atorvastatin should be prescribed with caution to patients with factors predisposing to the development of rhabdomyolysis. Before starting atorvastatin therapy, CPK activity in the blood plasma should be monitored in the following cases:
renal dysfunction,
· hypothyroidism,
· the patient has a history or family history of hereditary muscle disorders,
· already suffered toxic effects of HMG-CoA reductase inhibitors (statins) or fibrates on muscle tissue,
history of liver disease and/or patients who drink significant amounts of alcohol,
· in patients over the age of 70 years, the need to monitor CPK in the blood plasma should be assessed, given that these patients already have factors predisposing to the development of rhabdomyolysis,
· situations in which an increase in the concentration of atorvastatin in the blood plasma is expected, such as interactions with other drugs.
In such situations, the risk/benefit ratio should be assessed and medical monitoring of the patient’s condition should be carried out.
In case of a significant increase in serum CPK activity (more than 5 times the upper limit of normal), atorvastatin therapy should not be started.
When using the drug Atoris®, as well as other HMG-CoA reductase inhibitors, rare cases of rhabdomyolysis with acute renal failure caused by myoglobinuria have been described. A risk factor for the development of rhabdomyolysis may be pre-existing renal impairment. Such patients should be provided with more careful monitoring of the musculoskeletal system. If symptoms of myopathy appear or there are risk factors for the development of renal failure due to rhabdomyolysis (for example, severe acute infection, arterial hypotension, major surgery, trauma, metabolic, endocrine and fluid-electrolyte disturbances, uncontrolled convulsions), therapy with Atoris should be temporarily discontinued or completely discontinued.
Very rare cases of the development of immune-mediated necrotizing myopathy have been reported during therapy or upon discontinuation of statin use. Immune-mediated necrotizing myopathy is clinically characterized by persistent proximal muscle weakness and increased serum CPK activity that persist despite discontinuation of statin treatment.
Attention! Patients should be warned to seek immediate medical attention if they experience unexplained pain or muscle weakness, especially if accompanied by malaise or fever.
Prevention of stroke by actively reducing plasma cholesterol concentrations (SPARCL)
In a retrospective analysis of stroke subtypes, patients without coronary artery disease with a recent stroke or TIA initially treated with atorvastatin 80 mg had a higher incidence of hemorrhagic stroke compared with patients receiving placebo. The increased risk was particularly evident in patients with a history of hemorrhagic stroke or lacunar infarction at baseline. In this group of patients, the benefit/risk ratio when taking atorvastatin at a dose of 80 mg/day is not well defined; therefore, before starting therapy, the possible risk of hemorrhagic stroke in such patients should be carefully assessed.
After a special analysis of a clinical trial involving 4731 patients without coronary artery disease who had a stroke or TIA within the previous 6 months who were prescribed atorvastatin 80 mg/day, a higher incidence of hemorrhagic stroke was found in the atorvastatin 80 mg group compared with the placebo group (55 in the atorvastatin group vs. 33 in the placebo group). Patients with hemorrhagic stroke at the time of inclusion in the study had a higher risk of recurrent hemorrhagic stroke (7 in the atorvastatin group versus 2 in the placebo group). However, patients receiving atorvastatin 80 mg/day had fewer strokes of any type (265 vs. 311) and fewer cardiovascular events (123 vs. 204).
Diabetes mellitus
Some data suggest that HMG-CoA reductase inhibitors (statins) as a class may lead to elevated blood glucose concentrations, and some patients at high risk for diabetes may develop a hyperglycemic state that requires treatment, as in diabetes mellitus. However, this risk does not outweigh the benefits of therapy with HMG-CoA reductase inhibitors (statins) in terms of vascular risks, so this cannot be a reason to discontinue therapy. Patients at risk (fasting blood glucose concentration from 5.6 to 6.9 mmol/l, BMI > 30 kg/m2 body surface area, increased TG concentration in blood plasma, arterial hypertension) should be under medical supervision, including monitoring of biochemical blood parameters, in accordance with National recommendations.
Interstitial lung disease
During therapy with certain HMG-CoA reductase inhibitors (statins), especially during long-term therapy, isolated cases of interstitial lung disease have been reported. Shortness of breath, nonproductive cough, and deterioration in general health (fatigue, weight loss, and fever) may occur. If interstitial lung disease is suspected in a patient, atorvastatin therapy should be discontinued.
Endocrine function
When using HMG-CoA reductase inhibitors (statins), including atorvastatin, cases of increased HbA1 concentration and fasting blood glucose concentration were observed. However, the risk of hyperglycemia is lower than the degree of reduction in the risk of vascular complications while taking HMG-CoA reductase inhibitors (statins).
Use in children
In the 3-year study, there were no clinically significant effects on growth and puberty as measured by the Global Maturation and Development Assessment, Tanner Stage Assessment, and Height and Weight Measurements.
Special information on excipients
The drug Atoris® contains lactose and is therefore contraindicated in the following conditions: lactose intolerance, lactase deficiency, glucose-galactose malabsorption syndrome.
There is no data on the effect of Atoris® on the ability to drive vehicles and engage in potentially hazardous activities that require increased concentration and speed of psychomotor reactions. However, given the possibility of dizziness, caution should be exercised when performing these activities.
Active ingredient
Active ingredient
Atorvastatin
Composition
Composition
1 film-coated tablet, 10 mg/20 mg contains:
Core
Active ingredient:
Atorvastatin calcium 10.36 mg/20.72 mg, equivalent to atorvastatin 10.00 mg/20.00 mg
Excipients:
Povidone-K25, sodium lauryl sulfate, calcium carbonate, microcrystalline cellulose, lactose monohydrate, croscarmellose sodium, magnesium stearate
Film casing
Opadry IIHP 85F28751 white*
*Opadray IIHP 85F28751 white:
Polyvinyl alcohol, titanium dioxide (E171), macrogol-3000, talc
Pregnancy
Pregnancy
Atoris® is contraindicated during pregnancy.
Women of reproductive age should use adequate contraception during treatment. The use of Atoris® is contraindicated in women of childbearing age who do not use adequate methods of contraception.
Rare cases of congenital anomalies have been reported after fetal exposure to HMG-CoA reductase inhibitors (statins) in utero. Animal studies have shown toxic effects on reproductive function. Atoris® is contraindicated during breastfeeding. It is not known whether atorvastatin is excreted in breast milk. If it is necessary to prescribe the drug during lactation, breastfeeding must be stopped to avoid the risk of adverse events in infants.
Contraindications
Contraindications
· Hypersensitivity to any component of the drug.
Active liver disease or an increase in the activity of “liver” transaminases in the blood plasma of unknown origin by more than 3 times compared with the upper limit of normal.
· Pregnancy.
· Breastfeeding period.
· Women of childbearing age who are not using adequate methods of contraception.
· Age under 18 years (there is insufficient clinical data on the effectiveness and safety of the drug in this age group), with the exception of heterozygous familial hypercholesterolemia (use is contraindicated in children under 10 years of age).
· Simultaneous use with fusidic acid.
Therapy with antiviral drugs for hepatitis C virus (HCV) glecaprevir/pibrentasvir.
Lactase deficiency, lactose intolerance, glucose-galactose malabsorption syndrome, since Atoris® contains lactose.
Side Effects
Side Effects
Atoris® is usually well tolerated; adverse reactions are usually mild and transient.
Classification of the frequency of side effects recommended by the World Health Organization (WHO):
very common ≥ 1/10
often ≥ 1/100 to < 1/10
uncommon ≥ 1/1000 to < 1/100
rarely from ≥ 1/10000 to < 1/1000
very rare <1/10000
frequency unknown cannot be estimated from available data.
Infectious and parasitic diseases:
often: nasopharyngitis.
Blood and lymphatic system disorders:
rarely: thrombocytopenia.
Immune system disorders:
often: allergic reactions;
very rare: anaphylaxis.
Metabolic and nutritional disorders:
often: hyperglycemia;
uncommon: hypoglycemia, weight gain, anorexia;
frequency unknown: diabetes mellitus (incidence depends on the presence or absence of risk factors [fasting blood glucose concentration ≥ 5.6 mmol/l, body mass index [BMI] > 30 kg/m2 body surface area, elevated plasma TG concentrations, history of hypertension]).
Mental disorders:
infrequently: nightmares, insomnia;
frequency unknown: depression.
Nervous system disorders:
often: headache;
uncommon: dizziness, paresthesia, hypoesthesia, impaired taste perception, amnesia;
rarely: peripheral neuropathy;
frequency unknown: memory loss or decline.
Visual disorders:
uncommon: the appearance of a “veil” before the eyes;
rarely: visual impairment.
Hearing and labyrinth disorders:
uncommon: tinnitus;
very rare: hearing loss.
Disorders of the respiratory system, chest and mediastinal organs:
often: sore throat, nosebleeds;
frequency unknown: isolated cases of interstitial lung disease (usually with long-term use).
Digestive system disorders:
often: constipation, flatulence, dyspepsia, nausea, diarrhea;
uncommon: vomiting, abdominal pain, belching, pancreatitis, abdominal discomfort.
Disorders of the liver and biliary tract:
uncommon: hepatitis;
rarely: cholestasis.
Disorders of the skin and subcutaneous tissues:
uncommon: urticaria, skin itching, skin rash, alopecia;
rarely: angioedema, bullous rash, polymorphic exudative erythema (including Stevens-Johnson syndrome), toxic epidermal necrolysis (Lyell’s syndrome).
Musculoskeletal and connective tissue disorders:
often: myalgia, arthralgia, pain in the limbs, muscle cramps, swelling of the joints, back pain, musculoskeletal pain;
uncommon: neck pain, muscle weakness;
rarely: myopathy, myositis, rhabdomyolysis, tendinopathy (in some cases with tendon rupture), muscle rupture;
very rarely: lupus-like syndrome;
frequency unknown: immune-mediated necrotizing myopathy.
Renal and urinary tract disorders:
very rare: secondary renal failure.
Disorders of the genital organs and breast:
uncommon: impotence;
very rare: gynecomastia.
General disorders and disorders at the injection site:
uncommon: malaise, asthenic syndrome, chest pain, peripheral edema, fatigue, fever.
Laboratory and instrumental data:
often: abnormal results of liver tests (AST and ALT) in blood plasma, increased activity of serum creatine phosphokinase (CPK);
uncommon: leukocyturia;
frequency unknown: increased concentration of glycosylated hemoglobin (HbAl).
Children
Children aged 10 to 17 years treated with atorvastatin had an adverse event profile similar to that of placebo-treated patients, with infections being the most common adverse event in both groups, regardless of assessment of causality. In the 3-year study, there were no clinically significant effects on growth and puberty as measured by the Global Maturation and Development Assessment, Tanner Stage Assessment, and Height and Weight Measurements. The safety and tolerability profile in children was similar to the known safety profile of atorvastatin in adults.
The clinical safety database includes safety data for 520 children treated with atorvastatin, of which 7 patients were aged <6 years, 121 patients were aged 6 to 9 years, and 392 patients were aged 10 to 17 years. Based on available data, the incidence, type and severity of adverse reactions in children are similar to those in adults.
Overdose
Overdose
There is no specific antidote for the treatment of overdose with Atoris®. In case of overdose, symptomatic treatment should be provided as needed. Liver function tests should be performed and serum CPK activity should be monitored. Since atorvastatin actively binds to plasma proteins, hemodialysis is ineffective.
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C, in the original packaging.
Keep out of the reach of children.
Shelf life
Shelf life
2 years.
Do not use the drug after the expiration date.
Manufacturer
Manufacturer
KRKA dd Novo Mesto, Slovenia
Additional information
| Shelf life | 2 years. Do not use the drug after the expiration date. |
|---|---|
| Conditions of storage | At the temperature not more than 25 °С, in the original package. Keep out of reach of children. |
| Manufacturer | KRKA dd Novo mesto, Slovenia |
| Medication form | pills |
| Brand | KRKA dd Novo mesto |
Other forms…
Related products
Buy Atoris, 20 mg 90 pcs. with delivery to USA, UK, Europe and over 120 other countries.