No products in the cart.
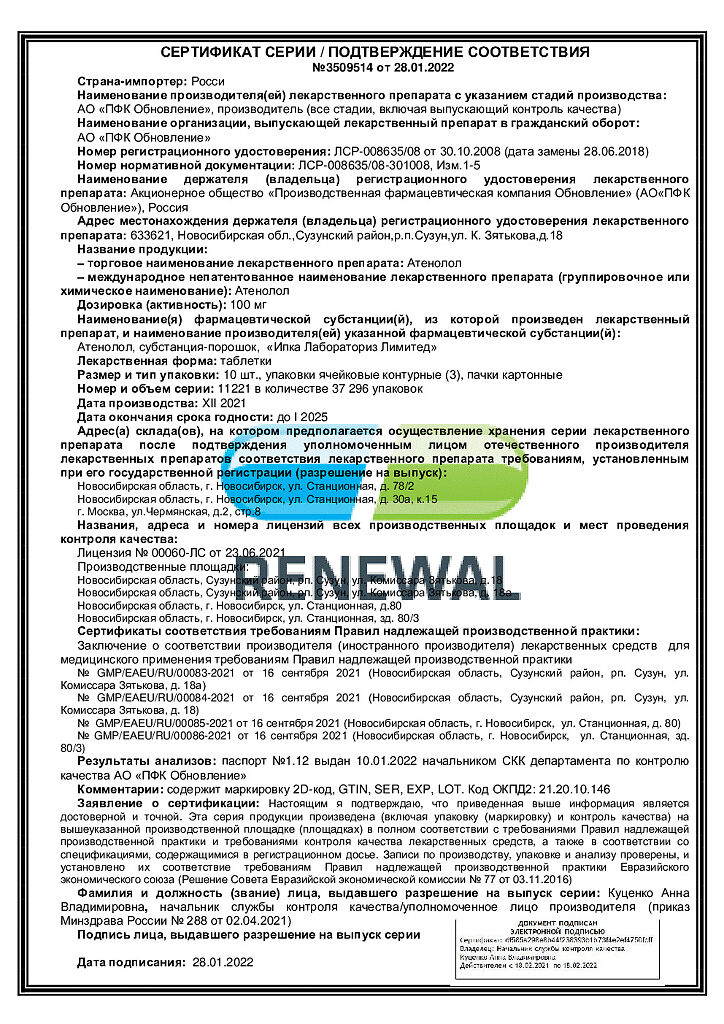
Atenolol, tablets 100 mg 30 pcs
€2.62 €2.18
Description
It has antianginal, antihypertensive and antiarrhythmic effects. It does not have membrane stabilizing and intrinsic sympathomimetic activity. Reduces catecholamine-stimulated formation of cAMP from ATP.
In the first 24 hours after oral administration against the background of decreased cardiac output there is reactive increase of total peripheral vascular resistance, which gradually decreases during 1-3 days.
The hypotensive effect is associated with decreased cardiac output, decreased activity of the renin-angiotensin system, baroreceptor sensitivity and influence on the central nervous system. Hypotensive effect is manifested by both reduction of systolic and diastolic blood pressure (BP), reduction of stroke and minute volumes.
In medium therapeutic doses, it has no effect on the tone of the peripheral arteries. Hypotensive effect lasts for 24 hours and with regular use is stabilized by the end of the second week of treatment.
The antianginal effect is determined by decrease of myocardial oxygen demand as a result of decrease of heart rate (prolongation of diastole and improvement of myocardial perfusion) and contractility and decrease of myocardial sensitivity to sympathetic stimulation. It reduces heart rate (HR) at rest and during physical activity.
By increasing left ventricular end-diastolic pressure and increasing ventricular muscle fiber stretch may increase oxygen demand, especially in patients with chronic heart failure.
The antiarrhythmic action is manifested by suppression of sinus tachycardia and is associated with the elimination of arrhythmogenic sympathetic effects on the cardiac conduction system, decreased rate of propagation of excitation through the sinoatrial node and prolongation of the refractory period.
It suppresses conduction of impulses in antegrade and, to a lesser extent, in retrograde direction through the AV (atrioventricular) node and through additional conduction pathways.
The negative chronotropic effect appears 1 h after administration, reaches a maximum after 2-4 h, lasts up to 24 h.
Decreases automatism of the sinus node, decreases HR, slows down AV conduction, decreases myocardial contractility, and decreases myocardial oxygen demand. Reduces myocardial excitability. When used in medium therapeutic doses, it has less effect on the smooth muscle of the bronchi and peripheral arteries than non-selective beta-adrenoblockers.
Pharmacokinetics
Absorption from the gastrointestinal tract is fast, incomplete (50-60%), bioavailability is 40-50%, time of reaching maximum concentration in plasma – 2-4 hours. It poorly penetrates through the blood-brain barrier, passes in small amounts through the placental barrier and into breast milk.
Binding with blood plasma proteins is 6-16%. It is practically unmetabolized in liver. Half-life is 6-9 hours (increased in elderly patients). It is excreted by kidneys through glomerular filtration (85-100% unchanged).
Renal dysfunction is accompanied by prolongation of the half-life and cumulation: with creatinine clearance below 35 ml/min/1.73 m2 the half-life is 16-27 h, with creatinine clearance below 15 ml/min/1.73 m2 – more than 27 h (dose reduction is necessary). It is excreted during hemodialysis.
Indications
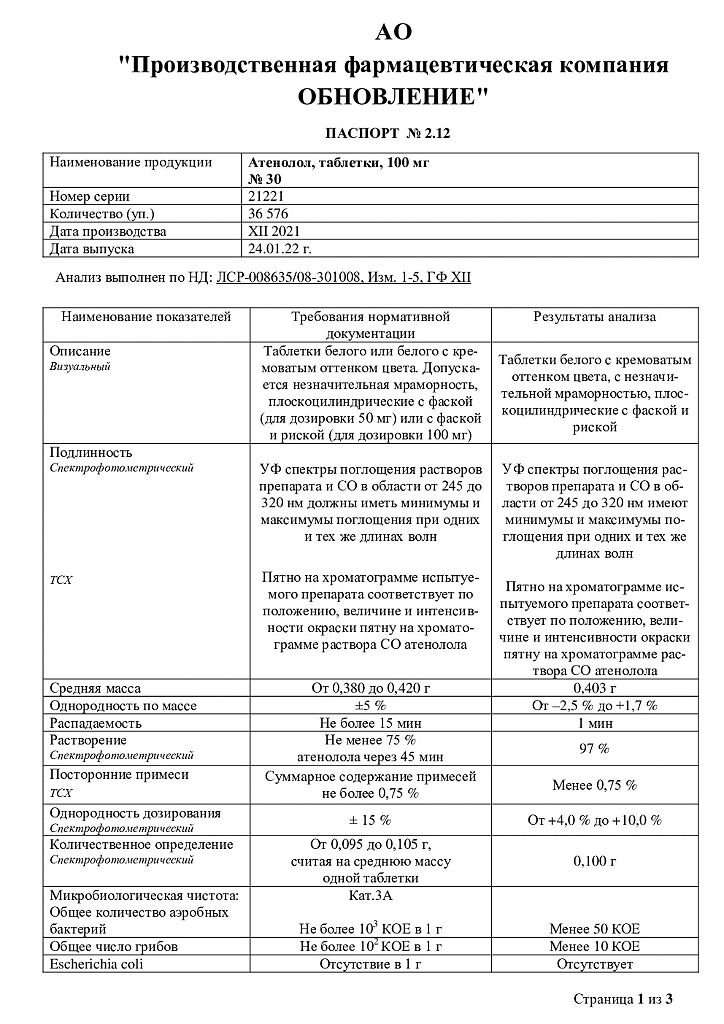
Indications
— Arterial hypertension;
– prevention of angina attacks (with the exception of Prinzmetal’s angina);
– heart rhythm disturbances: sinus tachycardia, prevention of supraventricular tachyarrhythmia, ventricular extrasystole.
Pharmacological effect
Pharmacological effect
It has antianginal, antihypertensive and antiarrhythmic effects. It does not have membrane stabilizing or internal sympathomimetic activity. Reduces the formation of cAMP from ATP stimulated by catecholamines.
In the first 24 hours after oral administration, against the background of a decrease in cardiac output, a reactive increase in total peripheral vascular resistance is observed, the severity of which gradually decreases over 1-3 days.
The hypotensive effect is associated with a decrease in cardiac output, a decrease in the activity of the renin-angiotensin system, baroreceptor sensitivity and an effect on the central nervous system. The hypotensive effect is manifested by both a decrease in systolic and diastolic blood pressure (BP), a decrease in stroke and cardiac output.
In average therapeutic doses it has no effect on the tone of peripheral arteries. The hypotensive effect lasts 24 hours, and with regular use it stabilizes by the end of the second week of treatment.
The antianginal effect is determined by a decrease in myocardial oxygen demand as a result of a decrease in heart rate (prolongation of diastole and improvement of myocardial perfusion) and contractility, as well as a decrease in the sensitivity of the myocardium to the effects of sympathetic stimulation. Reduces heart rate (HR) at rest and during physical activity.
By increasing end-diastolic pressure in the left ventricle and increasing the stretch of ventricular muscle fibers, it can increase oxygen demand, especially in patients with chronic heart failure.
The antiarrhythmic effect is manifested by suppression of sinus tachycardia and is associated with the elimination of arrhythmogenic sympathetic influences on the conduction system of the heart, a decrease in the rate of propagation of excitation through the sinoatrial node and an extension of the refractory period.
It inhibits the conduction of impulses in the antegrade and, to a lesser extent, in the retrograde directions through the AV (atrioventricular) node and along additional conduction pathways.
The negative chronotropic effect appears 1 hour after administration, reaches a maximum after 2-4 hours, and lasts up to 24 hours.
Reduces the automaticity of the sinus node, reduces heart rate, slows AV conduction, reduces myocardial contractility, and reduces myocardial oxygen demand. Reduces myocardial excitability. When used in average therapeutic doses, it has a less pronounced effect on the smooth muscles of the bronchi and peripheral arteries than non-selective
beta blockers.
Pharmacokinetics
Absorption from the gastrointestinal tract is rapid, incomplete (50-60%), bioavailability is 40-50%, time to reach maximum concentration in blood plasma is 2-4 hours. It penetrates poorly through the blood-brain barrier, passes in small quantities through the placental barrier and into breast milk.
Bonding with blood plasma proteins is 6-16%. Practically not metabolized in the liver. The half-life is 6-9 hours (increases in elderly patients). Excreted by the kidneys by glomerular filtration (85-100% unchanged).
Impaired renal function is accompanied by an extension of the half-life and cumulation: with creatinine clearance below 35 ml/min/1.73 m2, the half-life is 16-27 hours, with creatinine clearance below 15 ml/min/1.73 m2 – more than 27 hours (dosage reduction is necessary). It is excreted during hemodialysis.
Special instructions
Special instructions
Monitoring of patients taking atenolol should include monitoring heart rate and blood pressure (at the beginning of treatment – daily, then once every 3-4 months), blood glucose levels in patients with diabetes (once every 4-5 months). In elderly patients, it is recommended to monitor renal function (once every 4-5 months).
The patient should be taught how to calculate heart rate and instructed about the need for medical consultation if the heart rate is less than 50 beats/min. In thyrotoxicosis, atenolol may mask certain clinical signs of thyrotoxicosis (eg, tachycardia). Abrupt withdrawal in patients with thyrotoxicosis is contraindicated because it can increase symptoms. In diabetes mellitus, it can mask tachycardia caused by hypoglycemia. Unlike non-selective beta-blockers, it practically does not enhance insulin-induced hypoglycemia and does not delay the restoration of blood glucose to normal concentrations.
In patients with coronary heart disease (CHD), abrupt withdrawal of beta-blockers may cause an increase in the frequency or severity of anginal attacks, so discontinuation of atenolol in patients with CHD should be done gradually.
Compared with non-selective beta-blockers, cardioselective beta-blockers have less effect on pulmonary function, however, for obstructive airway diseases, atenolol is prescribed only when absolutely indicated. If it is necessary to prescribe them, in some cases the use of beta2-adrenergic agonists can be recommended.
Patients with bronchospastic diseases can be prescribed cardioselective adrenergic blockers in case of intolerance and/or ineffectiveness of other antihypertensive drugs, but the dosage should be strictly monitored. An overdose is dangerous due to the development of bronchospasm.
Particular attention is required in cases where surgical intervention under anesthesia is required in patients taking atenolol. The drug should be stopped 48 hours before the intervention. As an anesthetic, you should choose a drug with the least possible negative inotropic effect.
When using atenolol and clonidine simultaneously, atenolol should be discontinued several days before clonidine in order to avoid withdrawal symptoms from the latter. It is possible that the severity of the hypersensitivity reaction may increase and there will be no effect from usual doses of epinephrine against the background of a burdened allergic history.
Medicines that reduce catecholamine reserves (for example, reserpine) can enhance the effect of beta-blockers, so patients taking such combinations of drugs should be under constant medical supervision to detect a pronounced decrease in blood pressure or bradycardia.
If elderly patients develop increasing bradycardia (less than 50 beats/min), arterial hypotension (systolic blood pressure below 100 mm Hg), atrioventricular block, bronchospasm, ventricular arrhythmias, severe liver and kidney dysfunction, it is necessary to reduce the dose or stop treatment.
It is recommended to discontinue therapy if depression caused by taking beta-blockers develops.
If intravenous administration of verapamil is necessary, this should be done at least 48 hours after taking atenolol.
When using atenolol, it is possible to reduce the production of tear fluid, which is important in patients who use contact lenses.
Treatment should not be abruptly interrupted due to the risk of developing severe arrhythmias and myocardial infarction. Cancellation is carried out gradually, reducing the dose over 2 weeks. or more (reduce the dose by 25% in 3-4 days).
Should be discontinued before testing the content of catecholamines, normetanephrine and vanillylmandelic acid in the blood and urine; titers of antinuclear antibodies. Beta blockers are less effective in smokers. Pregnancy and lactation period.
Pregnant women should be prescribed atenolol only in cases where the benefit to the mother outweighs the potential risk to the fetus. Atenolol is excreted in breast milk, so if the drug is indicated during breastfeeding, it is better to stop breastfeeding for a while.
Impact on the ability to drive vehicles and operate machinery
During the treatment period, it is necessary to refrain from engaging in potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Active ingredient
Active ingredient
Atenolol
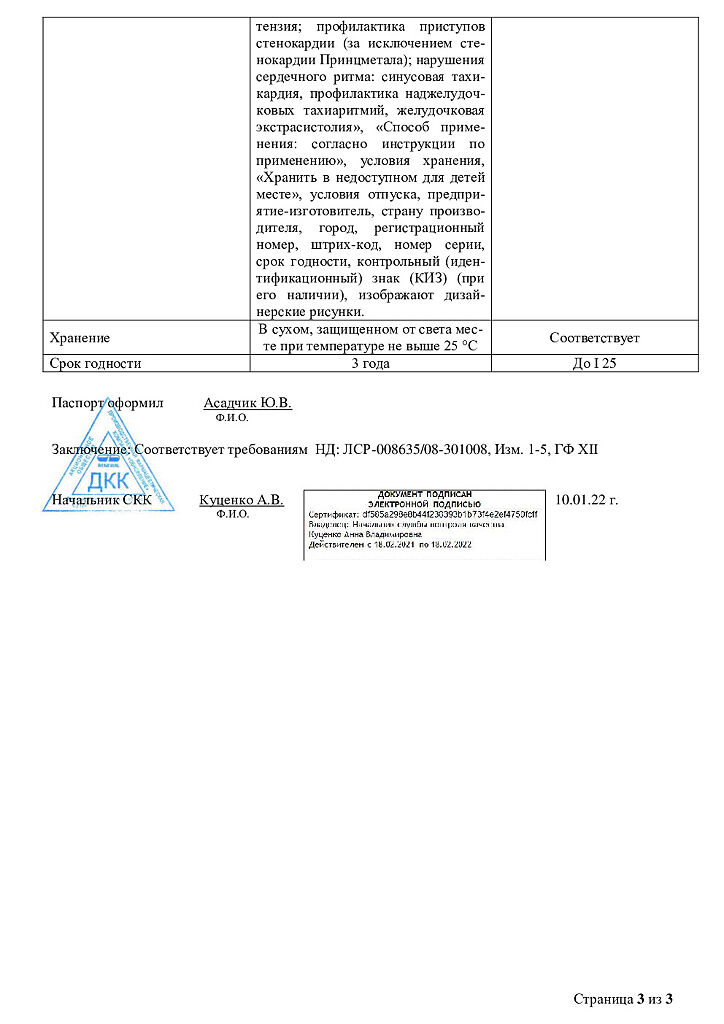
Composition
Composition
1 tablet contains:
active substance:
atenolol – 0.1 g
excipients:
magnesium hydroxycarbonate – 0.08 g – 0.16 g
potato starch – 0.059 g – 0.118 g
gelatin – 0.009 g – 0.018 g
magnesium stearate – 0.001 g – 0.002 g
stearic acid – 0.001 g – 0.002
Contraindications
Contraindications
— Cardiogenic shock;
— atrioventricular (AV) blockade II-III stage;
— severe bradycardia (heart rate less than 40 beats/min.);
— sick sinus syndrome;
– sinoauricular block;
– acute or chronic heart failure in the stage of decompensation;
– cardiomegaly without signs of heart failure;
– Prinzmetal’s angina;
– arterial hypotension (if used for myocardial infarction;
– systolic blood pressure less than 100 mm Hg);
– lactation period;
– simultaneous use of monoamine oxidase inhibitors (MAO);
– age under 18 years (the effectiveness and safety of the drug have not been established);
– hypersensitivity to the drug.
With caution: diabetes mellitus, metabolic acidosis, hypoglycemia, history of allergic reactions, chronic obstructive pulmonary disease (including emphysema), AV block of the first degree, chronic heart failure (compensated), obliterating peripheral vascular diseases (intermittent claudication, Raynaud’s syndrome), pheochromocytoma, liver failure, chronic renal disease failure, myasthenia gravis, thyrotoxicosis, depression (including a history), psoriasis, old age, pregnancy.
Side Effects
Side Effects
Cardiovascular system: development (worsening) of symptoms of chronic heart failure (swelling of the ankles, feet; shortness of breath), impaired atrioventricular conduction, arrhythmias, bradycardia, marked decrease in blood pressure, palpitations, weakening of myocardial contractility, orthostatic hypotension, manifestations of vasospasm (coldness of the lower extremities, Raynaud’s syndrome), vasculitis, pain in breasts
Central nervous system: dizziness, decreased ability to concentrate, decreased reaction speed, drowsiness or insomnia, depression, hallucinations, increased fatigue, headache, weakness, nightmares, anxiety, confusion or short-term memory loss, paresthesia in the limbs (in patients with intermittent claudication and Raynaud’s syndrome), muscle weakness, cramps.
Gastrointestinal tract: dry mouth, nausea, vomiting, diarrhea, abdominal pain, constipation or diarrhea, change in taste.
Respiratory system: dyspnea, bronchospasm, apnea, nasal congestion.
Hematological reactions: platelet purpura, anemia (aplastic), thrombosis.
Endocrine system: decreased potency, decreased libido, hyperglycemia (in patients with non-insulin-dependent diabetes mellitus), hypoglycemia (in patients receiving insulin), hypothyroid state.
Skin reactions: urticaria, dermatitis, itching, photosensitivity, increased sweating, skin hyperemia, exacerbation of psoriasis, reversible alopecia.
Sense organs: blurred vision, decreased secretion of tear fluid, dry and sore eyes, conjunctivitis.
Effect on the fetus: intrauterine growth retardation, hypoglycemia, bradycardia. Laboratory indicators: agranulocytosis, leukopenia, increased activity of liver enzymes, hyperbilirubinemia, thrombocytopenia (unusual bleeding and hemorrhage).
Other: back pain, arthrappia, withdrawal syndrome (tachycardia, increased frequency of angina attacks, increased blood pressure, etc.).
The frequency of side effects increases with increasing dosage of the drug.
Interaction
Interaction
With the simultaneous use of atenolol with insulin, hypoglycemic agents for oral administration, their hypoglycemic effect is enhanced. When used together with antihypertensive drugs of different groups or nitrates, the hypotensive effect is enhanced. Concomitant use of atenolol and verapamil (or diltiazem) may cause a mutually enhanced cardiodepressive effect.
The hypotensive effect is weakened by estrogens (sodium retention) and non-steroidal anti-inflammatory drugs, glucocorticosteroids. With the simultaneous use of atenolol and cardiac glycosides, the risk of developing bradycardia and atrioventricular conduction disorders increases.
When atenolol is prescribed simultaneously with reserpine, methyldopa, clonidine, verapamil, severe bradycardia may occur.
Simultaneous intravenous administration of verapamil and diltiazem can provoke cardiac arrest; nifedipine can lead to a significant decrease in blood pressure. When taking atenolol simultaneously with ergotamine and xanthine derivatives, its effectiveness is reduced.
When discontinuing the combined use of atenolol and clonidine, treatment with clonidine is continued for several more days after discontinuation of atenolol.
Concomitant use with lidocaine may reduce its elimination and increase the risk of lidocaine toxicity.
Use together with phenothiazine derivatives helps to increase the concentration of each drug in the blood serum.
Phenytoin, when administered intravenously, and drugs for general anesthesia (hydrocarbon derivatives) increase the severity of the cardiodepressive effect and the likelihood of a decrease in blood pressure.
When used together with aminophylline and theophylline, mutual suppression of therapeutic effects is possible.
Concomitant use with MAO inhibitors is not recommended due to a significant increase in the hypotensive effect; the break in treatment between taking MAO inhibitors and atenolol should be at least 14 days.
Allergens used for immunotherapy or allergen extracts used for skin testing increase the risk of severe systemic allergic reactions or anaphylaxis.
Inhalation anesthetics (hydrocarbon derivatives) increase the risk of suppression of myocardial function and the development of arterial hypertension. Amiodarone increases the risk of bradycardia and AV conduction depression. Cimetidine increases plasma concentrations (inhibits metabolism). Iodine-containing radiocontrast agents for intravenous administration increase the risk of anaphylactic reactions.
Prolongs the effect of non-depolarizing muscle relaxants and the anticoagulant effect of coumarins.
Tri- and tetracyclic antidepressants, antipsychotics (neuroleptics), ethanol, sedatives and hypnotics increase depression of the central nervous system.
Non-hydrogenated ergot alkaloids increase the risk of developing peripheral circulatory disorders.
Overdose
Overdose
Symptoms: severe bradycardia, AV block II-III degree, increasing symptoms of heart failure, excessive decrease in blood pressure, difficulty breathing, bronchospasm, dizziness, fainting, arrhythmia, ventricular extrasystole, cyanosis of fingernails or palms, convulsions.
Treatment: gastric lavage and administration of adsorbent drugs; if bronchospasm occurs, inhalation or intravenous administration of the beta2-adrenergic agonist salbutamol is indicated.
In case of impaired AV conduction, bradycardia – intravenous administration of 1-2 mg of atropine, epinephrine or installation of a temporary pacemaker; for ventricular extrasystole – lidocaine (class 1A drugs are not used); when blood pressure decreases, the patient should be in the Trendelenburg position.
If there are no signs of pulmonary edema – intravenous plasma replacement solutions, if ineffective – administration of epinephrine, dopamine, dobutamine; for chronic heart failure – cardiac glycosides, diuretics, glucagon; for convulsions – intravenous diazepam. Dialysis is possible.
Manufacturer
Manufacturer
Update of PFC JSC, Russia
Additional information
| Manufacturer | Update PFC AO, Russia |
|---|---|
| Medication form | pills |
| Brand | Update PFC AO |
Related products
Buy Atenolol, tablets 100 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.