No products in the cart.
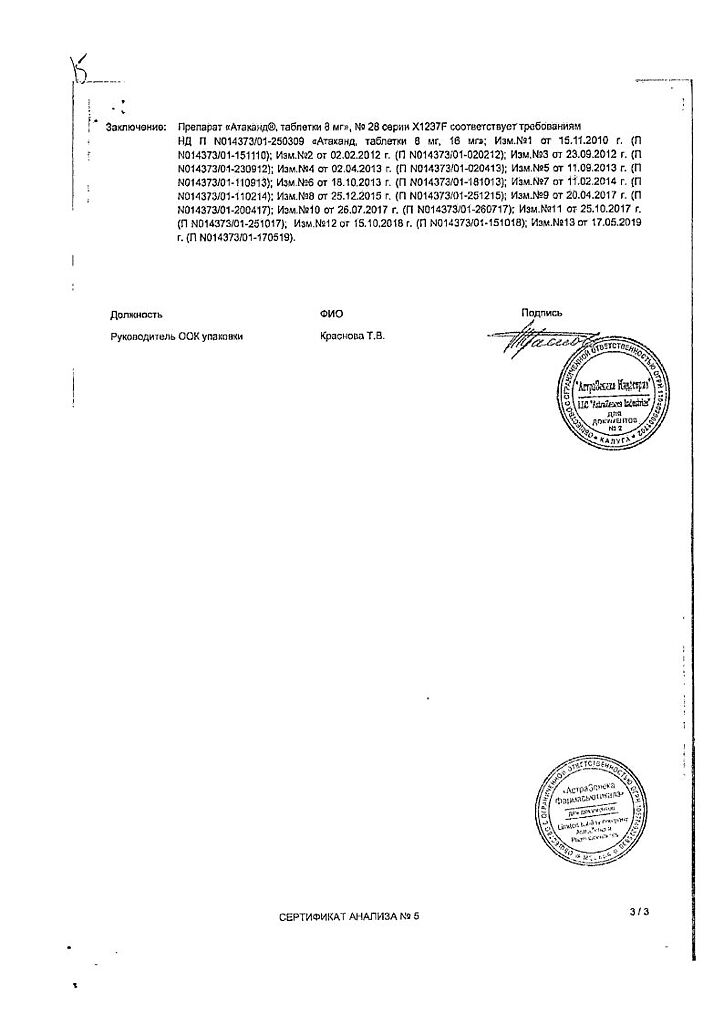
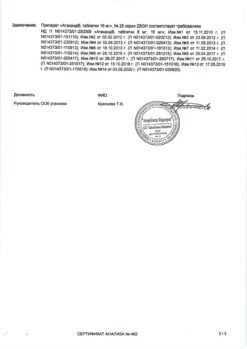
Atakand, tablets 8 mg 28 pcs.
€62.71 €52.26
Description
Pharmacotherapeutic group: Angiotensin II receptor antagonist.
ATX code: C09CA06
Pharmacological properties
Pharmacodynamics
Angiotensin II is the main hormone of the renin-angiotensin-aldosterone system, which plays an important role in the pathogenesis of arterial hypertension, heart failure and other cardiovascular diseases. The main physiological effects of angiotensin II are vasoconstriction, stimulation of aldosterone production, regulation of water-electrolyte homeostasis, and stimulation of cell growth. All these effects are mediated by interaction of angiotensin II with angiotensin type 1 receptors (AT1 receptors).
Candesartan is a selective angiotensin II type 1 receptor (AT1 receptor) antagonist. Candesartan does not inhibit angiotensin-converting enzyme (ACE), which converts angiotensin I to angiotensin II and degrades bradykinin; it does not affect ACE and does not lead to accumulation of bradykinin or substance P. When comparing candesartan with ACE inhibitors, cough development was less common in patients treated with candesartan cylexetil. Candesartan does not bind to other hormone receptors and does not block ion channels involved in the regulation of cardiovascular function. As a result of blocking of AT1 angiotensin II receptors, there is a dose-dependent increase of renin activity, angiotensin I and angiotensin II concentration and decrease of plasma aldosterone concentration.
Arterial hypertension
In arterial hypertension, candesartan causes a dose-dependent long-term decrease in blood pressure (BP).
The antihypertensive effect of the drug is due to a decrease in total peripheral vascular resistance, with no change in heart rate (HR). There have been no cases of marked arterial hypotension after the first dose of the drug, and no cases of withdrawal syndrome (ricochet syndrome) after discontinuation of therapy.
The beginning of antihypertensive effect after the first dose of candesartan cilexetil usually develops within 2 hours. On continued fixed-dose therapy with the drug, maximum BP reduction is usually achieved within 4 weeks and persists for the duration of treatment.
Candesartan cilexetil, administered once daily, provides an effective and gradual decrease in BP over 24 hours with little variation in BP between doses of the drug. The use of candesartan cilexetil together with hydrochlorothiazide leads to increased antihypertensive effect. Concomitant use of candesartan cilexetil and hydrochlorothiazide (or amlodipine) is well tolerated.
The efficacy of the drug is independent of the age and sex of patients.
Candesartan cilexetil increases renal blood flow and does not alter or increase glomerular filtration rate, whereas renal vascular resistance and filtration fraction decrease. Administration of candesartan cilexetil at a dose of 8-16 mg for 12 weeks has no adverse effect on glucose concentration and lipid profile in patients with arterial hypertension and type 2 diabetes.
. The clinical effects of candesartan cilexetil on morbidity and mortality when administered at a dose of 8-16 mg (mean dose 12 mg) once daily were examined in a randomized clinical trial involving 4,937 elderly patients (age 70 to 89 years, 21% of patients aged 80 years or older) with mild to moderate arterial hypertension receiving therapy with candesartan cilexetil for an average of 3.7 years (the SCOPE Study of Cognitive Function and Prognosis in Elderly Patients). Patients received candesartan cilexetil or placebo, if necessary, in combination with other hypotensive agents. Both regimens demonstrated efficacious reduction of systolic and diastolic BP (from 166/90 to 145/80 mmHg in candesartan-treated patients and from 167/90 to 149/82 mmHg in the control group) with good tolerability.
Cognitive function and quality of life were maintained at good levels in both patient groups. There were no statistically significant differences in the incidence of cardiovascular complications (cardiovascular mortality, rate of non-fatal myocardial infarction and non-fatal stroke) between the two patient groups.
In the group of patients receiving candesartan, there were 26.7 cardiovascular complications per 1000 patient-years compared with 30.0 cases per 1000 patient-years in the control group (relative risk=0.89, 95% confidence interval 0.75 to 1.06, p=0.19).
The table below shows the results of the primary endpoint (cardiovascular complications) and its components.
| Number of patients with a primary event | Relative risk (95% CI) | p | ||
| Candesartan cilexetil* (N=2477) | Control* (N=2460) | |||
| Cardiovascular complications | 242 | 268 | 0.19 | |
| – Cardiovascular mortality | 145 | 152 | 0.95 (0.75-1.19) | 0.63 |
| – Nonfatal stroke | 68 | td> 93 | 0.72 (0.53-0.99) | 0.04 |
| – Nonfatal myocardial infarction | 54 | 47 | 1.14 (0.77-1.68) | 0.52 |
* Prior to randomization, any prior antihypertensive therapy was standardized to hydrochlorothiazide at a dose of 12.5 mg once daily.
Another hypotensive agent was added to the double-blind study drug (candesartan cilexetil 8-16 mg or placebo once daily) if systolic BP remained ≥160 mm Hg and/or diastolic BP ≥90 mm Hg. Such additional therapy was received by 49% and 66% of patients in the candesartan cilexetil and control groups, respectively.
Cronic Heart Failure
The CHARM trial (Candesartan in Chronic Heart Failure – Assessment of Reduced Mortality and Morbidity) reported that use of candesartan cilexetil was associated with lower rates of death and need for hospitalization for chronic heart failure and improved left ventricular systolic function.
Patients with chronic heart failure received candesartan cilexetil at a dose of 4-8 mg per day in addition to basic therapy, with dose increases to 32 mg per day or to the maximum tolerated therapeutic dose (median dose of candesartan was 24 mg). The median duration of follow-up was 37.7 months. After 6 months of therapy, 63% of patients who continued to take candesartan cilexetil (89%) had a therapeutic dose of 32 mg.
The other CHARM-Alternative study (n=2028) included patients with reduced left ventricular ejection fraction (LVEF) ≤40% who were not receiving an ACE inhibitor due to intolerance (mainly due to coughing – 72%); rates of cardiovascular mortality and first hospitalization for chronic heart failure were significantly lower in patients receiving candesartan compared with the placebo group (hazard ratio = 0.77, 95% confidence interval 0.67 – 0.89, p In the CHARM-Added study (n = 2548), patients with decreased PVLD ≤40% receiving ACE inhibitors combined criterion, which included mortality from cardiovascular disease and first hospitalization for chronic heart failure, was significantly lower in the group of patients receiving candesartan compared with the placebo group (hazard ratio = 0.85, 95% confidence interval 0.75 to 0.96, p = 0.011), corresponding to a 15% reduction in relative risk.
In this study, 23 patients had to be treated throughout the study period to prevent one death from cardiovascular complications or hospitalization for chronic heart failure. The value of the combined efficacy criterion, which included an assessment of the incidence of death regardless of cause or the incidence of first hospitalization for chronic heart failure, was significantly lower in the group of patients receiving candesartan (hazard ratio = 0.87, 95% confidence interval 0.78 to 0.98, p = 0.021), which also indicated a positive effect with candesartan.
The use of candesartan cilexetil led to an improvement in the NYHA functional class of chronic heart failure (p=0.020).
In the CHARM-Preserve study (n=3023), patients with preserved systolic function (LVEF >40%), there were no statistically significant differences in the value of the combined efficacy criterion, which included the rate of death and the rate of first hospitalization for chronic heart failure, between the candesartan and placebo groups (hazard ratio = 0.89, 95% confidence interval 0.77 to 1.03, p = 0.118). The small numerical decrease in this criterion was due to a decrease in the frequency of hospitalizations for chronic heart failure. This study showed no effect of candesartan on mortality rates.
In a separate analysis of the 3 CHARM trials, there were no significant differences in mortality between the candesartan and placebo groups. However, mortality rates were estimated in the pooled population of the CHARM-Alternative and CHARM-Added trials and in all 3 trials (hazard ratio = 0.91, 95% confidence interval 0.83 to 1.00, p = 0.055). Reduced rates of death and hospitalizations for chronic heart failure on candesartan therapy were independent of age, sex, and concomitant therapy. Candesartan was also effective in patients taking beta-adreno-blockers in combination with ACE inhibitors, and the effectiveness of candesartan was independent of whether or not the patient was taking the optimal dose of ACE inhibitor.
In patients with chronic heart failure and reduced left ventricular systolic function (LVEF ≤40%), taking candesartan contributed to a decrease in total peripheral vascular resistance and pulmonary capillary pressure, increased renin activity and plasma angiotensin II concentration, and decreased aldosterone levels.
Pharmacokinetics
Intake and distribution
Candesartan cilexetil is a prodrug for oral administration. It rapidly converts to the active ingredient, candesartan, by ester hydrolysis upon absorption from the digestive tract, binds firmly to AT1 receptors and dissociates slowly, has no agonist properties.
The absolute bioavailability of candesartan after oral administration of candesartan cilexetil solution is approximately 40%.
The relative bioavailability of tablet versus oral solution is approximately 34%. Thus, the estimated absolute bioavailability of the tablet form of the drug is 14%. Maximum serum concentration (Cmax) is reached 3-4 hours after taking the tablet form of the drug. When increasing the dose of the drug within the recommended limits, the concentration of candesartan increases linearly.
The pharmacokinetic parameters of candesartan are independent of patient gender.
Eating has no significant effect on the area under the “concentration-time curve” (AUC), i.e. simultaneous eating does not significantly affect the bioavailability of the drug. Candesartan is actively bound to plasma proteins (>99%). The volume of distribution of candesartan is 0.1 l/kg.
Metabolism and excretion
Candesartan is mainly excreted unchanged by the kidneys and bile and only to a minor extent is metabolized in the liver. The elimination half-life of candesartan is approximately 9 hours. Cumulation in the body is not observed.
The total clearance of candesartan is approximately 0.37 ml/min/kg, with a renal clearance of approximately 0.19 ml/min/kg. Renal excretion of candesartan is by glomerular filtration and active tubular secretion. When administered orally, radioactively labeled candesartan cilexetil is excreted by the kidneys about 26% of the administered amount as candesartan and 7% as an inactive metabolite, while 56% of the administered amount is found in the feces as candesartan and 10% as an inactive metabolite.
In elderly patients (older than 65 years), the Cmax and AUC of candesartan are increased by 50% and 80%, respectively, compared to younger patients. However, the hypotensive effect and the incidence of side effects with Atacand® do not depend on the age of patients.
In patients with mild to moderate renal impairment, the Cmax and AUC of candesartan were increased by 50% and 70%, respectively, while the half-life of the drug was unchanged compared to patients with normal renal function. In patients with severe renal impairment, the Cmax and AUC of candesartan increased by 50% and 110%, respectively, while the half-life of the drug was doubled. Patients on hemodialysis showed similar pharmacokinetic parameters for candesartan as patients with severe renal impairment.
In patients with mild to moderate hepatic impairment, there was a 23% increase in the AUC of candesartan.
Indications
Indications
Arterial hypertension
Chronic heart failure and impaired left ventricular systolic function (decrease in LVEF ≤40%) as additional therapy to angiotensin-converting enzyme (ACE) inhibitors or in case of intolerance to ACE inhibitors
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: angiotensin II receptor antagonist.
ATX code: C09CA06
Pharmacological properties
Pharmacodynamics
Angiotensin II is the main hormone of the renin-angiotensin-aldosterone system, which plays an important role in the pathogenesis of arterial hypertension, heart failure and other cardiovascular diseases. The main physiological effects of angiotensin II are vasoconstriction, stimulation of aldosterone production, regulation of water-electrolyte homeostasis and stimulation of cell growth. All these effects are mediated by the interaction of angiotensin II with angiotensin type 1 receptors (AT1 receptors).
Candesartan is a selective antagonist of angiotensin II type 1 receptors (AT1 receptors). Candesartan does not inhibit angiotensin-converting enzyme (ACE), which converts angiotensin I to angiotensin II and destroys bradykinin; does not affect ACE and does not lead to the accumulation of bradykinin or substance P. When comparing candesartan with ACE inhibitors, the development of cough was less common in patients receiving candesartan cilexetil. Candesartan does not bind to the receptors of other hormones and does not block ion channels involved in the regulation of the functions of the cardiovascular system. As a result of blocking the AT1 receptors of angiotensin II, there is a dose-dependent increase in renin activity, the concentration of angiotensin I, angiotensin II and a decrease in the concentration of aldosterone in the blood plasma.
Arterial hypertension
In arterial hypertension, candesartan causes a dose-dependent, long-term decrease in blood pressure (BP).
The antihypertensive effect of the drug is due to a decrease in total peripheral vascular resistance, without changing heart rate (HR). There were no cases of severe arterial hypotension after taking the first dose of the drug, as well as withdrawal syndrome (rebound syndrome) after cessation of therapy.
The onset of antihypertensive effect after taking the first dose of candesartan cilexetil usually develops within 2 hours. With continued therapy with the drug at a fixed dose, the maximum reduction in blood pressure is usually achieved within 4 weeks and is maintained throughout treatment.
Candesartan cilexetil, prescribed once a day, provides an effective and smooth decrease in blood pressure over 24 hours with minor fluctuations in blood pressure in the intervals between doses of the drug. The use of candesartan cilexetil in combination with hydrochlorothiazide leads to an enhanced antihypertensive effect. The combined use of candesartan cilexetil and hydrochlorothiazide (or amlodipine) is well tolerated.
The effectiveness of the drug does not depend on the age and gender of patients.
Candesartan cilexetil increases renal blood flow and does not change or increases glomerular filtration rate, while renal vascular resistance and filtration fraction are reduced. Taking candesartan cilexetil at a dose of 8-16 mg for 12 weeks does not have a negative effect on glucose concentrations and lipid profiles in patients with arterial hypertension and type 2 diabetes mellitus.
The clinical effects of candesartan cilexetil on morbidity and mortality when administered at a dose of 8-16 mg (mean dose 12 mg) once daily were investigated in a randomized clinical trial involving 4937 elderly patients (ages 70 to 89 years, 21% of patients aged 80 years or older) with mild to moderate hypertension receiving candesartan therapy cilexetil for an average of 3.7 years (SCOPE study – a study of cognitive function and prognosis in elderly patients). Patients received candesartan cilexetil or placebo, if necessary, in combination with other antihypertensive agents. Both treatment regimens showed an effective reduction in systolic and diastolic blood pressure (from 166/90 to 145/80 mmHg in the group of patients receiving candesartan, and from 167/90 to 149/82 mmHg in the control group) and were well tolerated.
Cognitive function and quality of life remained at a good level in both groups of patients. There were no statistically significant differences in the incidence of cardiovascular events (cardiovascular mortality, nonfatal myocardial infarction, and nonfatal stroke) between the two groups of patients.
In the candesartan group, there were 26.7 incident cardiovascular events per 1000 patient-years compared with 30.0 per 1000 patient-years in the control group (relative risk = 0.89, 95% confidence interval 0.75 to 1.06, p = 0.19).
The table below presents the results of the assessment of the primary end point (cardiovascular complications) and its components.
Number of patients with primary event
Relative risk (95% CI)
p
Candesartan cilexetil* (N=2477)
Control* (N=2460)
Cardiovascular complications
242
268
0.89 (0.75-1.06)
0.19
– Cardiovascular mortality
145
152
0.95 (0.75-1.19)
0.63
– Non-fatal stroke
68
93
0.72 (0.53-0.99)
0.04
– Non-fatal myocardial infarction
54
47
1.14 (0.77-1.68)
0.52
*Before randomization, any previous antihypertensive therapy was standardized to hydrochlorothiazide at a dose of 12.5 mg once daily.
Another antihypertensive agent was added to the double-blind study drug (candesartan cilexetil 8–16 mg or placebo once daily) if systolic BP remained ≥160 mmHg and/or diastolic BP ≥90 mmHg. 49% and 66% of patients in the candesartan cilexetil group and control group, respectively, received such additional therapy.
Chronic heart failure
According to the results of the CHARM (Candesartan in Chronic Heart Failure – Mortality and Morbidity Reduction Assessment) study, the use of candesartan cilexetil led to a reduction in the incidence of death and the need for hospitalization for chronic heart failure and to an improvement in left ventricular systolic function.
Patients with chronic heart failure, in addition to the main therapy, received candesartan cilexetil at a dose of 4-8 mg per day with a dose increase to 32 mg per day or to the maximum tolerated therapeutic dose (the average dose of candesartan was 24 mg). The median follow-up duration was 37.7 months. After 6 months of therapy, 63% of patients continuing to take candesartan cilexetil (89%) received a therapeutic dose of 32 mg.
Another study, the CHARM-Alternative study (n=2028), included patients with reduced left ventricular ejection fraction (LVEF) ≤40% who did not receive an ACE inhibitor due to intolerance (mainly cough – 72%); The rates of cardiovascular death and first hospitalization for chronic heart failure were significantly lower in the candesartan group compared with the placebo group (hazard ratio = 0.77, 95% confidence interval 0.67 – 0.89, p In the CHARM-Added study (n = 2548) in patients with reduced LVEF ≤40% receiving ACE inhibitors, The composite measure of cardiovascular mortality and first hospitalization for chronic heart failure was significantly lower in the candesartan group compared with the placebo group (hazard ratio = 0.85, 95% confidence interval 0.75 – 0.96, p = 0.011), corresponding to a 15% reduction in relative risk.
In this study, to prevent one cardiovascular death or hospitalization for chronic heart failure, it was necessary to treat 23 patients throughout the study period. The value of the combined effectiveness criterion, which included an assessment of the incidence of deaths regardless of their cause or the frequency of the first hospitalization for chronic heart failure, was significantly lower in the group of patients receiving candesartan (risk ratio = 0.87, 95% confidence interval 0.78 – 0.98, p = 0.021), which also indicated a positive effect with the use of candesartan.
The use of candesartan cilexetil led to an improvement in the functional class of chronic heart failure according to the NYHA classification (p = 0.020).
In the CHARM-Preserve study (n=3023), in patients with preserved systolic function (LVEF >40%), there were no statistically significant differences in the combined efficacy criterion, which included the incidence of death and the incidence of first hospitalization for chronic heart failure, in the candesartan and placebo groups (hazard ratio = 0.89, 95% confidence interval 0.77 – 1.03, p = 0.118). The small numerical decrease in this criterion was due to a decrease in the frequency of hospitalizations for chronic heart failure. This study did not show the effect of candesartan on the incidence of deaths.
When separately analyzing the results of 3 studies of the CHARM program, there were no significant differences in the incidence of deaths in the candesartan and placebo groups. However, the incidence of death was estimated in the pooled population of the CHARM-Alternative and CHARM-Added studies and in all 3 studies (hazard ratio = 0.91, 95% confidence interval 0.83 – 1.00, p = 0.055). The reduction in the incidence of deaths and hospitalizations for chronic heart failure during candesartan therapy was independent of age, gender and concomitant therapy. Candesartan was also effective in patients taking beta-blockers in combination with ACE inhibitors, and the effectiveness of candesartan was independent of whether the patient was taking the optimal dose of the ACE inhibitor or not.
In patients with chronic heart failure and reduced left ventricular systolic function (LVEF ≤40%), taking candesartan helped reduce total peripheral vascular resistance and capillary pressure in the lungs, increase renin activity and the concentration of angiotensin II in the blood plasma, as well as reduce aldosterone levels.
Pharmacokinetics
Suction and distribution
Candesartan cilexetil is an oral prodrug. It quickly turns into the active substance – candesartan through ether hydrolysis when absorbed from the digestive tract, binds strongly to AT1 receptors and slowly dissociates, does not have agonist properties.
The absolute bioavailability of candesartan after oral administration of candesartan cilexetil solution is about 40%.
The relative bioavailability of the tablet preparation compared to the oral solution is approximately 34%. Thus, the calculated absolute bioavailability of the tablet form of the drug is 14%. The maximum concentration in the blood serum (Cmax) is achieved 3-4 hours after taking the tablet form of the drug. With an increase in the dose of the drug within the recommended limits, the concentration of candesartan increases linearly.
The pharmacokinetic parameters of candesartan do not depend on the gender of the patient.
Food intake does not have a significant effect on the area under the concentration-time curve (AUC), i.e. simultaneous food intake does not significantly affect the bioavailability of the drug. Candesartan actively binds to plasma proteins (>99%). The volume of distribution of candesartan is 0.1 l/kg.
Metabolism and excretion from the body
Candesartan is mainly excreted unchanged from the body by the kidneys and bile and is only slightly metabolized in the liver. The half-life of candesartan is approximately 9 hours. Cumulation in the body is not observed.
The total clearance of candesartan is about 0.37 ml/min/kg, while the renal clearance is about 0.19 ml/min/kg. Renal excretion of candesartan is carried out by glomerular filtration and active tubular secretion. When radiolabeled candesartan cilexetil is administered orally, approximately 26% of the administered amount is excreted by the kidneys as candesartan and 7% as an inactive metabolite, whereas 56% of the administered amount is found in the feces as candesartan and 10% as an inactive metabolite.
In elderly patients (over 65 years of age), the Cmax and AUC of candesartan increase by 50% and 80%, respectively, compared to young patients. However, the hypotensive effect and the incidence of side effects when using the drug Atacand® do not depend on the age of the patients.
In patients with mild and moderate renal impairment, the Cmax and AUC of candesartan increased by 50% and 70%, respectively, while the half-life of the drug did not change compared to patients with normal renal function. In patients with severe renal impairment, the Cmax and AUC of candesartan increased by 50% and 110%, respectively, and the half-life of the drug increased by 2 times. In patients on hemodialysis, the same pharmacokinetic parameters of candesartan were found as in patients with severe renal impairment.
In patients with mild to moderate hepatic impairment, the AUC of candesartan increased by 23%.
Special instructions
Special instructions
When prescribing Atacand to patients with renal artery stenosis (bilateral or single artery stenosis), it should be taken into account that drugs that affect the renin-angiotensin-aldosterone system (ACE inhibitors) may increase the concentration of urea and creatinine in the blood serum. There is a possibility (unconfirmed) that similar effects may be observed with the use of angiotensin II antagonists.
Patients receiving hydrochlorothiazide at a dose of 12.5 mg tolerated subsequent use of Atacand at a dose of 8 mg. Patients also tolerate simultaneous therapy with hydrochlorothiazide at a dose of up to 25 mg and Atacand at a dose of 8-16 mg for 8 weeks. However, with a pronounced decrease in blood volume (when diuretics are used in high doses), symptomatic hypotension may occur, which is also typical for other drugs that affect the renin-angiotensin-aldosterone system. Obviously, this condition must be corrected before using Atacand.
Concomitant use of Atacand with potassium-sparing diuretics that do not remove potassium from the body can theoretically lead to an increase in serum potassium concentrations. Caution should be exercised if this combination is necessary.
Use in pediatrics
The clinical effectiveness and safety of Atacand in children has not been established.
Active ingredient
Active ingredient
Candesartan
Composition
Composition
Active substance:
candesartan cilexetil 8 mg.
Excipients:
Carmellose calcium (carmellose calcium salt) 5.6 mg,
hyprolose (hydroxypropyl cellulose) 4.0 mg,
iron dye red oxide E 172 0.065 mg;
lactose monohydrate 89.4 mg,
magnesium stearate 0.4 mg,
corn starch 20.0 mg,
macrogol 2.6 mg.
Pregnancy
Pregnancy
The drug is contraindicated for use during pregnancy.
Experimental studies have found that the use of candesartan leads to impaired renal function in the fetus in late stages of development, as well as in the neonatal period. The mechanism of this action is probably related to the effect of the drug on the renin-angiotensin-aldosterone system.
In humans, fetal renal perfusion, which depends on the state of the renin-angiotensin-aldosterone system, begins in the second trimester of pregnancy. Thus, the risk to the fetus increases when taking the drug in the second trimester.
It has not been established whether candesartan is excreted in breast milk. If it is necessary to use the drug during lactation, breastfeeding should be stopped due to the potential for the development of negative side effects in the child.
In experimental studies, candesartan was found in the milk of lactating rats.
Contraindications
Contraindications
Hypersensitivity to candesartan cilexetil or other components included in the drug.
Pregnancy and breastfeeding (see section “Use during pregnancy and breastfeeding”).
Severe liver dysfunction and/or cholestasis.
Age up to 18 years (efficacy and safety have not been established).
Lactose intolerance, lactase deficiency and glucose-galactose malabsorption syndrome.
The use of candesartan cilexetil in combination with drugs containing aliskiren in patients with diabetes mellitus (type 1 or 2) or with moderate or severe renal failure (glomerular filtration rate <60 ml/min/1.73 m²).
With caution: in patients with severe renal failure (creatinine clearance less than 30 ml/min), bilateral renal artery stenosis or stenosis of the artery of a single kidney, with hemodynamically significant stenosis of the aortic and mitral valve, after a history of kidney transplantation, in patients with cerebrovascular diseases and coronary heart disease (CHD), hyperkalemia, in patients with reduced circulating blood volume, with primary hyperaldosteronism (there is not enough data from clinical studies), hypertrophic obstructive cardiomyopathy.
Side Effects
Side Effects
From the side of the central nervous system: often (more than 2%) – headache, dizziness.
From laboratory parameters: increased AST activity (slightly higher than in the groups taking placebo). In general, no clinically significant changes in laboratory parameters were detected when taking Atacand.
Other: often (more than 2%) – back pain.
Clinical trials revealed that the drug was well tolerated; the incidence of side effects was comparable to placebo and did not depend on the dose of the drug, as well as on the age and gender of the patient. In general, side effects were moderate and temporary. The number of cases of drug discontinuation due to side effects was similar to the number in the group of patients taking candesartan cilexetil and placebo.
The cause-and-effect relationship between taking Atacand and the described side effects has not been established.
Interaction
Interaction
Interaction with other drugs and other forms of drug interactions
Pharmacokinetic studies examined the combined use of Atacand with hydrochlorothiazide, warfarin, digoxin, oral contraceptives (ethinyl estradiol/levonorgestrel), glibenclamide, nifedipine and enalapril. No clinically significant drug interactions were identified.
Candesartan is metabolized in the liver to a small extent (CYP2C9). Interaction studies have not revealed any effect of the drug on CYP2C9 and CYP3A4; the effect on other isoenzymes of the cytochrome P450 system has not been studied.
The combined use of Atacand with other antihypertensive drugs potentiates the hypotensive effect.
Experience with other drugs acting on the renin-angiotensin-aldosterone system shows that concomitant therapy with potassium-sparing diuretics, potassium supplements, salt substitutes containing potassium, and other drugs that can increase serum potassium levels (for example, heparin) can lead to the development of hyperkalemia.
When lithium preparations were combined with ACE inhibitors, a reversible increase in the concentration of lithium in the blood serum and the development of toxic reactions were reported. Similar reactions may also occur with the use of angiotensin II receptor antagonists, and therefore it is recommended to monitor serum lithium levels when using these drugs in combination.
The bioavailability of candesartan is independent of food intake.
Overdose
Overdose
Symptoms
Analysis of the pharmacological properties of the drug suggests that the main manifestation of an overdose may be a clinically significant decrease in blood pressure and dizziness. Isolated cases of drug overdose (up to 672 mg of candesartan cilexetil) have been described, resulting in the recovery of patients without serious consequences.
Treatment
With the development of clinically significant arterial hypotension, it is necessary to carry out symptomatic treatment and monitor the patient’s condition. Lay the patient down and raise the head of the bed. If necessary, the volume of circulating plasma should be increased, for example, by intravenous administration of an isotonic sodium chloride solution. If necessary, sympathomimetic drugs can be prescribed. Elimination of candesartan by hemodialysis is unlikely.
Storage conditions
Storage conditions
At temperatures below 30 °C
Shelf life
Shelf life
3 years
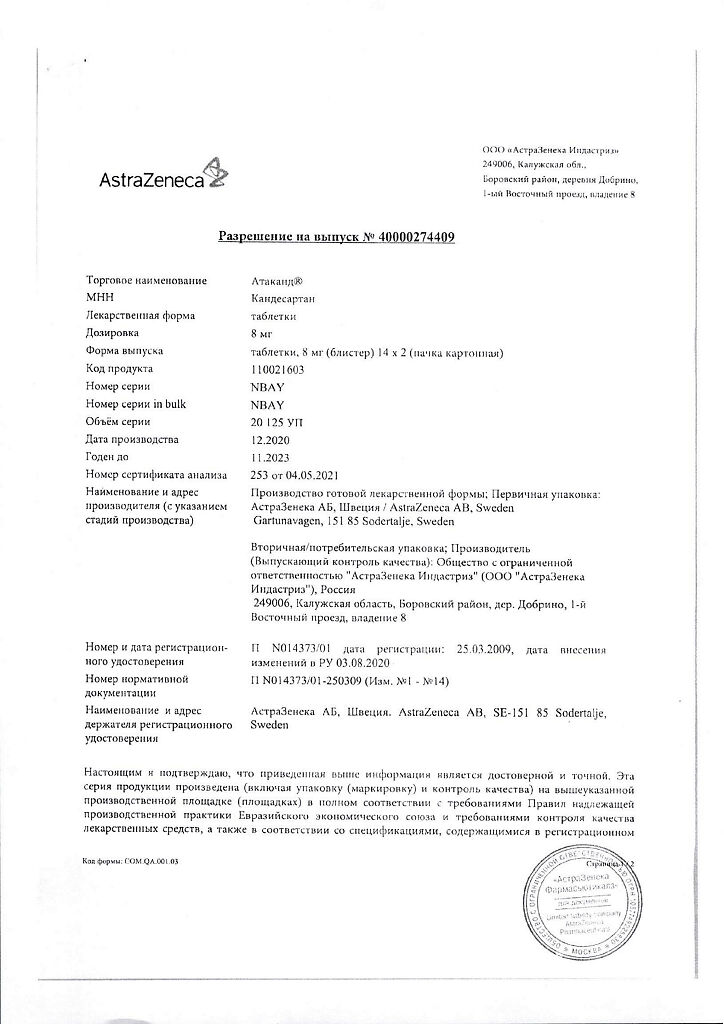
Manufacturer
Manufacturer
AstraZeneca AB, Sweden
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | At temperatures below 30 °C |
| Manufacturer | AstraZeneca AB, Sweden |
| Medication form | pills |
| Brand | AstraZeneca AB |
Other forms…
Related products
Buy Atakand, tablets 8 mg 28 pcs. with delivery to USA, UK, Europe and over 120 other countries.