No products in the cart.
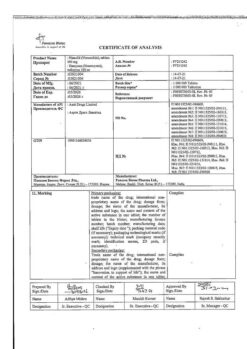
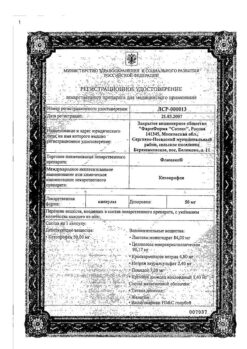
Artrosan, 6 mg/ml 2.5 ml 10 pcs.
€1.00
Out of stock
(E-mail when Stock is available)
Description
Pharmacotherapeutic group:nonsteroidal anti-inflammatory drug
ATX code: M01AC06
Pharmacological properties.
Pharmacodynamics
Meloxicam is a non-steroidal anti-inflammatory drug, refers to enolic acid derivatives and has anti-inflammatory, analgesic and antipyretic effects.The pronounced anti-inflammatory effect of meloxicam was established in all standard models of inflammation. The mechanism of action of meloxicam lies in its ability to inhibit the synthesis of prostaglandins – known mediators of inflammation. Meloxicam inhibits the synthesis of prostaglandins at the site of inflammation to a greater extent than in the gastric mucosa or kidneys.
These differences are associated with a more selective inhibition of cyclooxygenase-2 (COX-2) compared to cyclooxygenase-1 (COX-1). Inhibition of COX-2 is thought to provide the therapeutic actions of NSAIDs, whereas inhibition of the ever-present iso-enzyme COX-1 may be responsible for gastric and renal side effects. The selectivity of meloxicam against COX-2 has been confirmed in various test systems, both in-vitro and in-vivo. The selective ability of meloxicam to inhibit COX-2 was shown when using human whole blood in-vitro as a test system.Meloxicam (at doses of 7.5 and 15 mg) was found to be more active in inhibiting COX-2, having a greater inhibitory effect on lipopolysaccharide-stimulated prostaglandin E2 production (COX-2-controlled response) than on thromboxane production involved in blood clotting (COX-1-controlled response).These effects were dose-dependent.In exvivo studies, meloxicam (at doses of 7.5 mg and 15 mg) was shown to have no effect on platelet aggregation and bleeding time.
In clinical studies, gastrointestinal (GI) side effects were generally less frequent with meloxicam 7.5 and 15 mg than with the other NSAIDs compared. This difference in the frequency of gastrointestinal side effects is mainly due to the fact that such phenomena as dyspepsia, vomiting, nausea, and abdominal pain were observed less frequently while taking meloxicam. The frequency of upper gastrointestinal perforations, ulcers and bleeding associated with meloxicam use was low and depended on the size of the drug dose.
Pharmacokinetics
Absorption
Meloxicam is completely absorbed after intramuscular administration. The relative bioavailability compared to the bioavailability with oral administration is almost 100%. Therefore, no dose adjustment is required when switching from injectable to oral forms. After administering 15 mg of the drug intramuscularly, the peak plasma concentration (about 1.6-1.8 µg/ml), is reached within approximately 60 to 96 minutes.
Distribution
Meloxicam binds very well to plasma proteins, mainly to albumin (99%). It penetrates the synovial fluid, the concentration in the synovial fluid is about 50% of the plasma concentration. The volume of distribution is low, approximately 11 liters. Individual differences are 7 – 20%.
Metabolism
Meloxicam is almost completely metabolized in the liver to form 4 pharmacologically inactive derivatives. The main metabolite, 5-carboxymeloxicam (60% of the dose value), is formed by oxidation of an intermediate metabolite, 5- hydroxymethylmeloxicam, which is also excreted, but to a lesser extent (9% of the dose value). In-vitro studies have shown that CYP2C9 isoenzyme plays an important role in this metabolic transformation, CYP3A4 isoenzyme has additional importance. Peroxidase, which activity probably varies individually, takes part in formation of two other metabolites (which are 16% and 4% of drug dose, respectively).
Elimation
Elimated equally through intestine and kidneys, mainly as metabolites. Less than 5% of daily dose is excreted unchanged in the feces, the drug is excreted unchanged in the urine only in trace amounts. Mean elimination half-life of meloxicam varies from 13 to 25 hours.
Plasma clearance averages 7-12 ml/min after a single use.
Meloxicam demonstrates linear pharmacokinetics at doses of 7.5-15 mg when administered intramuscularly.
Inadequate hepatic and/or renal function
Inadequate hepatic function and mild renal insufficiency have no significant effect on the pharmacokinetics of meloxicam. The elimination rate of meloxicam from the body is significantly higher in patients with moderately severe renal insufficiency. Meloxicam binds less well with plasma proteins in patients with terminal renal failure. In terminal renal failure, increased volume of distribution may lead to higher concentrations of free meloxicam, so in these patients the daily dose should not exceed 7.5 mg.
Elderly patients
Elderly patients compared to younger patients have similar pharmacokinetic parameters. Elderly patients have slightly lower mean plasma clearance during equilibrium pharmacokinetics than younger patients. Elderly women have higher AUC values (area under the concentration-time curve) and a longer half-life compared to younger patients of both sexes.
In elderly patients, the average plasma clearance during the equilibrium state of pharmacokinetics is slightly lower than in younger patients.
Indications
Indications
Initial therapy and short-term symptomatic treatment for:
– osteoarthritis (arthrosis, degenerative joint diseases);
– rheumatoid arthritis;
– ankylosing spondylitis;
– other inflammatory and degenerative diseases of the musculoskeletal system, such as arthropathy, dorsopathies (for example, sciatica, low back pain, shoulder periarthritis and others), accompanied by pain.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: non-steroidal anti-inflammatory drug
ATC code: M01AC06
Pharmacological properties
Pharmacodynamics
Meloxicam is a non-steroidal anti-inflammatory drug, belongs to enolic acid derivatives and has anti-inflammatory, analgesic and antipyretic effects. The pronounced anti-inflammatory effect of meloxicam has been established in all standard models of inflammation. The mechanism of action of meloxicam is its ability to inhibit the synthesis of prostaglandins, known mediators of inflammation. Meloxicaminvivo inhibits the synthesis of prostaglandins at the site of inflammation to a greater extent than in the gastric mucosa or kidneys.
These differences are associated with more selective inhibition of cyclooxygenase-2 (COX-2) compared to cyclooxygenase-1 (COX-1). Inhibition of COX-2 is thought to mediate the therapeutic effects of NSAIDs, whereas inhibition of the constitutively present isoenzyme COX-1 may be responsible for gastric and renal side effects. The selectivity of meloxicam for COX-2 has been confirmed in various test systems, both invitro and invivo. The selective ability of meloxicam to inhibit COX-2 was shown when using human whole blood as a test system in vitro. It was found that meloxicam (in doses of 7.5 and 15 mg) more actively inhibited COX-2, having a greater inhibitory effect on the production of prostaglandin E2, stimulated by lipopolysaccharide (reaction controlled by COX-2), than on the production of thromboxane, which is involved in the process blood clotting (a response controlled by COX-1). These effects were dose-dependent. In exvivo studies, meloxicam (at doses of 7.5 mg and 15 mg) has no effect on platelet aggregation and bleeding time.
In clinical studies, gastrointestinal (GIT) side effects were generally less common with meloxicam 7.5 and 15 mg than with other NSAIDs compared. This difference in the frequency of side effects from the gastrointestinal tract is mainly due to the fact that when taking meloxicam, such phenomena as dyspepsia, vomiting, nausea, and abdominal pain were observed less frequently. The incidence of upper gastrointestinal perforations, ulcers and bleeding associated with the use of meloxicam was low and depended on the dose of the drug.
Pharmacokinetics
Absorption
Meloxicam is completely absorbed after intramuscular administration. Relative bioavailability compared to oral bioavailability is almost 100%. Therefore, when switching from injection to oral forms, dose selection is not required. After administration of 15 mg of the drug intramuscularly, peak plasma concentration (about 1.6-1.8 μg/ml) is achieved within approximately 60-96 minutes.
Distribution
Meloxicam binds very well to plasma proteins, mainly albumin (99%). Penetrates into synovial fluid, the concentration in synovial fluid is approximately 50% of the concentration in plasma. The volume of distribution is low, approximately 11 L. Individual differences are 7 – 20%.
Metabolism
Meloxicam is almost completely metabolized in the liver with the formation of 4 pharmacologically inactive derivatives. The main metabolite, 5-carboxymeloxicam (60% of the dose), is formed by oxidation of the intermediate metabolite, 5-hydroxymethylmeloxicam, which is also excreted, but to a lesser extent (9% of the dose). In vitro studies have shown that the CYP2C9 isoenzyme plays an important role in this metabolic transformation; the CYP3A4 isoenzyme is of additional importance. Peroxidase is involved in the formation of the other two metabolites (constituting, respectively, 16% and 4% of the drug dose), the activity of which probably varies individually.
Withdrawal
Excreted equally through the intestines and kidneys, mainly in the form of metabolites. Less than 5% of the daily dose is excreted unchanged in feces; the drug is found unchanged in urine only in trace amounts. The average half-life of meloxicam varies from 13 to 25 hours.
Plasma clearance averages 7-12 ml/min after a single dose.
Meloxicam exhibits linear pharmacokinetics in doses of 7.5-15 mg when administered intramuscularly.
Failure of liver and/or kidney function
Failure of liver function, as well as mild renal failure, do not have a significant effect on the pharmacokinetics of meloxicam. The rate of elimination of meloxicam from the body is significantly higher in patients with moderate renal failure. Meloxicam binds less well to plasma proteins in patients with end-stage renal failure. In end-stage renal failure, increased volume of distribution may result in higher concentrations of free meloxicam, so in these patients the daily dose should not exceed 7.5 mg.
Elderly patients
Elderly patients compared to young patients have similar pharmacokinetic parameters. In elderly patients, the average plasma clearance during steady-state pharmacokinetics is slightly lower than in younger patients. Elderly women have higher AUC (area under the concentration-time curve) values and a longer half-life compared to younger patients of both sexes.
Special instructions
Special instructions
The drug can change the properties of platelets, but does not replace the preventive effect of acetylsalicylic acid in cardiovascular diseases.
Caution should be exercised when using the drug in patients with a history of gastric and duodenal ulcers, and in patients on anticoagulant therapy. Such patients have an increased risk of erosive and ulcerative diseases of the gastrointestinal tract.
Caution should be exercised and monitoring of daily diuresis and renal function when using the drug in the elderly and patients with reduced circulating blood volume and reduced glomerular filtration (dehydration, chronic heart failure, cirrhosis of the liver, nephrotic syndrome, clinically significant kidney disease, taking diuretics, dehydration after major surgery).
If signs of liver damage appear (itching, yellowing of the skin, nausea, vomiting, abdominal pain, dark urine, persistent and significant increase in transaminase levels and changes in other indicators of liver function), the drug should be stopped and consulted with your doctor.
After two weeks of using the drug, it is necessary to monitor the activity of liver enzymes.
In patients with a slight or moderate decrease in renal function (creatinine clearance > 30 ml/min), no dose adjustment is required.
Patients taking diuretics and meloxicam simultaneously should take sufficient fluids.
If allergic reactions occur (itching, skin rash, urticaria, photosensitivity) during treatment, you should consult a doctor to decide whether to stop taking the drug.
Meloxicam, like other NSAIDs, can mask the symptoms of infectious diseases.
The use of meloxicam, like other drugs that block prostaglandin synthesis, can affect fertility and is therefore not recommended for women planning pregnancy.
The drug should not be used simultaneously with other NSAIDs. Impact on the ability to drive vehicles and machinery
No special clinical studies have been conducted on the effect of the drug on the ability to drive a car or use machinery. However, the possibility of dizziness and drowsiness, visual impairment and other disorders of the central nervous system should be taken into account. During treatment, patients must be careful when driving vehicles and engaging in other activities that require increased concentration and reaction speed.
Active ingredient
Active ingredient
Meloxicam
Composition
Composition
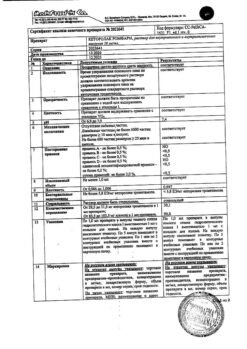
Active substance: Meloxicam – 6.00 mg
Excipients: meglumine – 3.75 mg, poloxamer 188 – 50.00 mg, tetrahydrofurfurylmacrogol (glycofurol) – 100.00 mg, glycine – 5.00 mg, sodium chloride – 3.00 mg, 1 M sodium solution hydroxide – up to pH 8.2-8.9, water for injection – up to 1 ml.
One ampoule (2.5 ml) contains 15 mg of meloxicam.
Pregnancy
Pregnancy
The use of Artrosan® is contraindicated during pregnancy.
It is known that NSAIDs pass into breast milk, therefore the use of Artrosan® during breastfeeding is contraindicated.
As a drug that inhibits cyclooxygenase/prostaglandin synthesis, meloxicam may affect fertility and is therefore not recommended for women planning pregnancy. Meloxicam may delay ovulation. In this regard, in women who have problems conceiving and are undergoing examination for such problems, it is recommended to stop taking the drug.
Contraindications
Contraindications
– Hypersensitivity to the active ingredient or auxiliary components of the drug;
– Hypersensitivity (including to other non-steroidal anti-inflammatory drugs).
Complete or incomplete combination of bronchial asthma, recurrent polyposis of the nose and paranasal sinuses, angioedema or urticaria caused by intolerance to acetylsalicylic acid or other non-steroidal anti-inflammatory drugs due to the existing likelihood of cross-sensitivity (including a history);
– Erosive and ulcerative lesions of the stomach and duodenum in the acute stage or recently suffered;
– Inflammatory bowel diseases – Crohn’s disease or ulcerative colitis in the acute stage;
– Severe liver and heart failure;
– Severe renal failure (if hemodialysis is not performed, creatinine clearance is less than 30 ml/min, and also with confirmed hyperkalemia);
– Active liver disease;
– Active gastrointestinal bleeding, recent cererevascular bleeding or an established diagnosis of diseases of the blood coagulation system;
– Age up to 18 years;
– Pregnancy;
– Breastfeeding period;
– Therapy of perioperative pain during coronary artery bypass surgery;
– Concomitant therapy with anticoagulants, as there is a risk of intramuscular hematomas;
With caution
– history of gastrointestinal tract diseases (presence of Helicobacter pylori infection);
– congestive heart failure;
– renal failure (creatinine clearance 30-60 ml/min);
– coronary heart disease;
– cerebrovascular diseases;
– dyslipidemia/hyperlipidemia;
– diabetes mellitus;
– concomitant therapy with anticoagulants, oral glucocorticosteroids, antiplatelet agents, selective serotonin reuptake inhibitors;
– diseases of peripheral arteries;
– old age;
– long-term use of NSAIDs;
– smoking;
– frequent consumption of alcohol.
Side Effects
Side Effects
The following describes side effects that were considered possible to be associated with the use of meloxicam.
Side effects recorded during post-marketing use, the relationship of which was assessed as possible with the use of meloxicam, are marked with a *.
Within systemic organ classes, the following categories are used according to the frequency of side effects:
very often (≥ 1/10);
often (≥ 1/100. < 1/10);
uncommon (≥ 1/ 1,000. < 1/100);
rare (≥ 1/10,000.< 1/1,000);
very rare (< 1/10,000);
not installed.
From the blood and lymphatic system:
Uncommon – anemia;
Rarely – leukopenia, thrombocytopenia, changes in the number of blood cells, including changes in the leukocyte formula.
Immune system disorders:
Uncommon – other immediate hypersensitivity reactions*
Not established – anaphylactic shock*, anaphylactoid reactions.
Mental disorders:
Rarely – mood changes*;
Not established – confusion*, disorientation*.
From the nervous system:
Often – headache;
Uncommon: dizziness, drowsiness
From the organs of vision, hearing and labyrinthine disorders:
Uncommon: vertigo;
Rarely – conjunctivitis*, visual disturbances, including blurred vision*, tinnitus.
From the heart and blood vessels:
Uncommon – increased blood pressure, a feeling of a “rush” of blood to the face; Rarely – palpitations;
Respiratory system disorders:
Rarely – bronchial asthma in patients with allergies to acetylsalicylic acid and other NSAIDs.
Gastrointestinal disorders:
Often – dyspepsia, abdominal pain, diarrhea, nausea, vomiting;
Uncommon – hidden or obvious gastrointestinal bleeding, gastritis*, stomatitis, constipation, bloating, belching;
Rarely – gastroduodenal ulcers, colitis, esophagitis;
Very rarely – perforation of the gastrointestinal tract
Disorders of the liver and biliary tract:
Infrequently, transient changes in liver function parameters (for example, increased transaminase or bilirubin activity);
Very rarely – hepatitis*.
Disorders of the skin and subcutaneous tissues:
Uncommon: itching, skin rash, angioedema*;
Rarely – urticaria, toxic epidermal necrolysis*, Stevens-Johnson syndrome*;
Very rarely – bullous dermatitis*, erythema multiforme*;
Not established – photosensitivity.
From the kidneys and urinary tract:
Uncommon: changes in renal function (increased creatinine and/or urea levels in the blood serum), urinary disorders, including acute urinary retention*;
Very rarely – acute renal failure*.
General disorders and disorders at the injection site:
Often – pain and swelling at the injection site;
Uncommon: swelling
Concomitant use with drugs that suppress bone marrow (for example, methotrexate) may cause cytopenia.
Gastrointestinal bleeding, ulceration, or perforation can be fatal.
As with other NSAIDs, the possibility of interstitial nephritis, glomerulonephritis, renal medullary necrosis, and nephrotic syndrome cannot be excluded.
Interaction
Interaction
– Other prostaglandin synthesis inhibitors, including glucocorticoids and salicylates – simultaneous use with meloxicam increases the risk of ulcers in the gastrointestinal tract and gastrointestinal bleeding (due to synergistic action). and are therefore not recommended. Concomitant use with other NSAIDs is not recommended.
– Anticoagulants for oral administration, heparin for systemic use, thrombolytic agents – simultaneous use with meloxicam increases the risk of bleeding. In case of simultaneous use, careful monitoring of the blood coagulation system is necessary.
– Antiplatelet drugs, serotonin reuptake inhibitors – simultaneous use with meloxicam increases the risk of bleeding due to inhibition of platelet function. In case of simultaneous use, careful monitoring of the blood coagulation system is necessary
– Lithium preparations – NSAIDs increase the concentration of lithium in plasma by reducing its excretion by the kidneys. The simultaneous use of meloxicam with lithium preparations is not recommended. If simultaneous use is necessary, careful monitoring of plasma lithium concentrations is recommended throughout the course of lithium preparations.
– Methotrexate – NSAIDs reduce the secretion of methotrexate by the kidneys, thereby increasing its plasma concentration. Concomitant use of eloxicam and methotrexate (at a dose of more than 15 mg per week) is not recommended. In case of simultaneous use, careful monitoring of renal function and blood count is necessary. Meloxicam may increase the hematological toxicity of methotrexate, especially in patients with impaired renal function.
– Contraception – there is evidence that NSAIDs may reduce the effectiveness of intrauterine contraceptive devices, but this has not been proven.
– Diuretics – the use of NSAIDs in case of dehydration of patients is accompanied by the risk of developing acute renal failure.
– Antihypertensive drugs (beta-blockers, angiotensin-converting enzyme inhibitors, vasodilators, diuretics). NSAIDs reduce the effect of antihypertensive drugs due to inhibition of prostaglandins, which have vasodilating properties.
– Angiotensin-II receptor antagonists, as well as angiotensin-converting enzyme inhibitors, when used together with NSAIDs, increase the decrease in glomerular filtration, which can thereby lead to the development of acute renal failure, especially in patients with impaired renal function.
– Cholestyramine, by binding meloxicam in the gastrointestinal tract, leads to its faster elimination.
– Pemetrexed – when meloxicam and pemetrexed are used concomitantly in patients with a clearance of 45 to 79 ml/min, meloxicam should be discontinued five days before starting pemetrexed and can be resumed 2 days after the end of use. If concomitant use of meloxicam and pemetrexed is necessary, such patients should be closely monitored, especially with regard to myelosuppression and the occurrence of gastrointestinal side effects. In patients with creatinine clearance less than 45 ml/min, taking meloxicam with pemetrexed is not recommended.
NSAIDs, by acting on renal prostaglandins, may increase the nephrotoxicity of cyclosporine.
When using drugs with meloxicam that are known to inhibit CYP 2C9 and/or CYP 3A4 (or are metabolized by these enzymes), such as sulfonylureas or probenecid, the possibility of pharmacokinetic interaction should be taken into account. When used together with oral antidiabetic agents (eg, sulfonylureas, nateglinide), interactions mediated by CYP 2C9 are possible, which may lead to increased concentrations of both these drugs and meloxicam in the blood. Patients taking meloxicam concomitantly with a sulfonylurea or nateglinide should carefully monitor their blood sugar levels due to the possibility of hypoglycemia.
With the simultaneous use of antacids, cimetidine, digoxin and furosemide, no significant pharmacokinetic interactions were identified.
Overdose
Overdose
Insufficient data have been accumulated on cases involving drug overdose. Symptoms characteristic of NSAID overdose are likely to be present in severe cases:
drowsiness, disturbances of consciousness, nausea, vomiting, epigastric pain, gastrointestinal bleeding, acute renal failure, changes in blood pressure, respiratory arrest, asystole.
Treatment: no known antidote. In case of drug overdose, symptomatic therapy should be used. Colestyramine is known to accelerate the elimination of meloxicam.
Storage conditions
Storage conditions
In a place protected from light at a temperature not exceeding 25°C.
Keep out of the reach of children.
Shelf life
Shelf life
5 years.
Manufacturer
Manufacturer
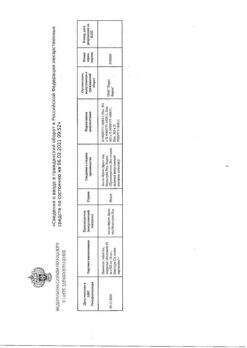
Pharmstandard-UfaVITA, Russia
Additional information
| Shelf life | 5 years. |
|---|---|
| Conditions of storage | Store in a place protected from light at a temperature not exceeding 25°C. Keep out of reach of children. |
| Manufacturer | Pharmstandard-UfaVITA, Russia |
| Medication form | solution |
| Brand | Pharmstandard-UfaVITA |
Other forms…
Related products
Buy Artrosan, 6 mg/ml 2.5 ml 10 pcs. with delivery to USA, UK, Europe and over 120 other countries.