No products in the cart.
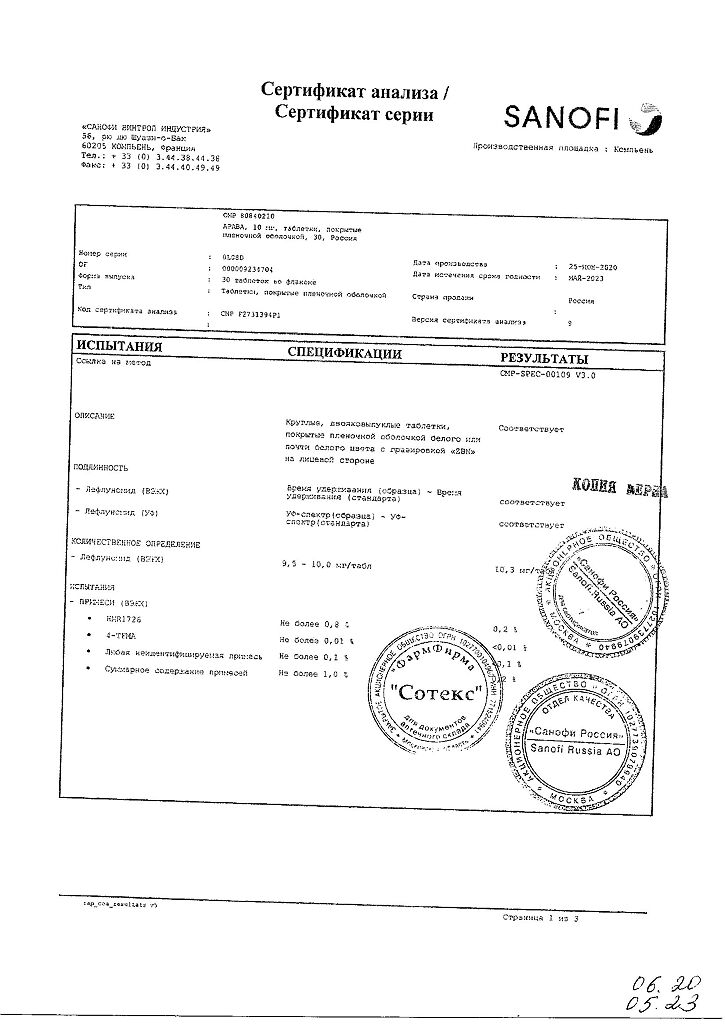
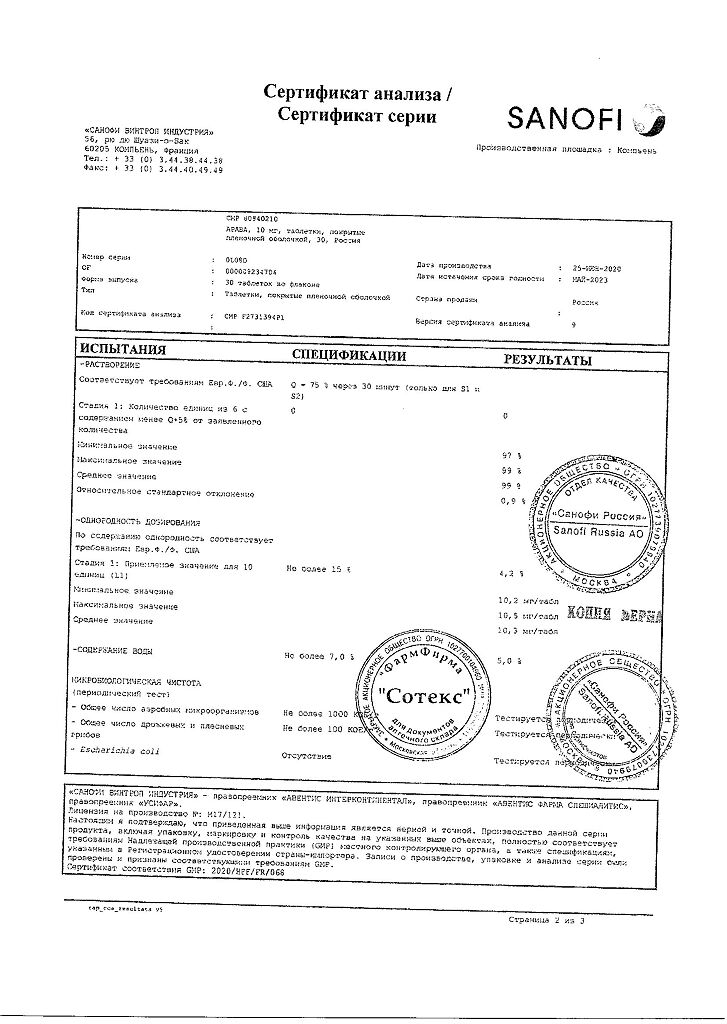
Arava, 10 mg 30 pcs.
€31.77 €26.47
Out of stock
(E-mail when Stock is available)
Description
Pharmacological action:
Arava belongs to the class of basic antirheumatic drugs and has antiproliferative, immunomodulatory, immunosuppressive and anti-inflammatory properties. The active metabolite of leflunomide A771726 inhibits the enzyme dehydrorotate dehydrogenase and has antiproliferative activity. Under in vitro conditions A771726 inhibits mitogen-induced proliferation and DNA synthesis of T-lymphocytes.
The antiproliferative activity of A771726 appears to be manifested at the level of pyrimidine biosynthesis, since the addition of uridine to the cell culture eliminates the inhibitory effect of the metabolite A771726. Using radioisotope ligands, it was shown that A771726 selectively binds to the enzyme dehydrorotate dehydrogenase, which explains its ability to inhibit this enzyme and lymphocyte proliferation at the G1 stage.
Lymphocyte proliferation is one of the key steps in the development of rheumatoid arthritis.
At the same time, A771726 inhibits the expression of interleukin-2 receptors (CB-25) and Ki-67 and PCNA cell-cycle-related core antigens.
Therapeutic effects of leflunomide have been shown in several experimental models of autoimmune diseases, including rheumatoid arthritis.
Leflunomide reduces symptoms and slows the progression of joint damage in the active form of rheumatoid arthritis.
The therapeutic effect is usually seen after 4-6 weeks and may build up further over a period of 4-6 months.
Indications
Indications
As a basic treatment for adult patients with active rheumatoid arthritis in order to reduce symptoms of the disease and delay the development of structural damage to the joints.
Active form of psoriatic arthritis.
Pharmacological effect
Pharmacological effect
Pharmaceutical action:
Arava belongs to the class of basic antirheumatic drugs and has antiproliferative, immunomodulatory, immunosuppressive and anti-inflammatory properties. The active metabolite of leflunomide A771726 inhibits the enzyme dehydroorotate dehydrogenase and has antiproliferative activity. A771726 inhibits mitogen-induced proliferation and DNA synthesis of T lymphocytes in vitro.
The antiproliferative activity of A771726 appears to manifest itself at the level of pyrimidine biosynthesis, since the addition of uridine to the cell culture eliminates the inhibitory effect of the A771726 metabolite. Using radioisotope ligands, it was shown that A771726 selectively binds to the enzyme dehydroorotate dehydrogenase, which explains its ability to inhibit this enzyme and the proliferation of lymphocytes at the G1 stage.
Lymphocyte proliferation is one of the key stages in the development of rheumatoid arthritis.
At the same time, A771726 inhibits the expression of receptors for interleukin-2 (CB-25) and nuclear antigens Ki-67 and PCNA, associated with the cell cycle.
The therapeutic effects of leflunomide have been demonstrated in several experimental models of autoimmune diseases, including rheumatoid arthritis.
Leflunomide reduces symptoms and slows the progression of joint damage in active rheumatoid arthritis.
The therapeutic effect usually appears after 4-6 weeks and can further increase over 4-6 months.
Special instructions
Special instructions
Arava should only be prescribed to patients after a thorough medical examination.
Before starting treatment with Arava, it is necessary to remember about the possible increase in the number of side effects in patients who have previously received other basic drugs for the treatment of rheumatoid arthritis, which have hepato- and hematotoxic effects.
The active metabolite of leflunomide, A771726, has a long half-life, usually ranging from 1 to 4 weeks. Due to the long half-life of leflunomide’s active metabolite, A771726, serious adverse effects (e.g., hepatotoxicity, hematoxicity, or allergic reactions, see below) may occur or persist even if leflunomide treatment is discontinued. In this case, a “washing” procedure should be carried out. The procedure can be repeated according to clinical indications. If severe immunological/allergic reactions such as Stevens-Johnson syndrome or Lyell’s syndrome are suspected, a complete “washing” procedure is mandatory.
Therefore, if such cases of toxicity occur or when switching to another basic drug (for example, methotrexate) after treatment with leflunomide, it is necessary to carry out a washout procedure (see below).
Liver reactions
Because the active metabolite of leflunomide, A771726, is protein bound and eliminated through hepatic metabolism and bile secretion, it is expected that plasma levels of A771726 may be increased in patients with hypoproteinemia. Arava is contraindicated in patients with severe hypoproteinemia or impaired liver function. (see section “Contraindications”.).
Rare cases of severe liver damage, in some cases fatal, have been reported during treatment with leflunomide. Most of these cases were observed during the first six months of treatment. Although the causal relationship of these adverse events to leflunomide has not been established, and in most cases there were several additional suspicious factors, strict adherence to treatment monitoring recommendations is considered mandatory.
ALT levels should be checked before starting leflunomide therapy and then every 2 weeks for the first 6 months of treatment, followed by once every 6 to 8 weeks.
There are the following recommendations for adjusting the dosage regimen or discontinuing the drug, depending on the severity and persistence of the increase in ALT levels.
If ALT is confirmed to be 2-3 times the upper limit of normal, reducing the dose from 20 mg to 10 mg per day may allow leflunomide to be continued, provided that this indicator is carefully monitored.
If 2-3 times the upper limit of normal ALT persists, or if there is a confirmed rise in ALT levels greater than 3 times the upper limit of normal, leflunomide should be discontinued and a washout procedure should be initiated.
Due to possible additive hepatotoxic effects, it is recommended to avoid alcohol intake during treatment with leflunomide.
Hematological reactions
A complete clinical blood count, including determination of the leukocyte formula and platelet count, should be performed before starting treatment with leflunomide, as well as every 2 weeks during the first 6 months of treatment and then every 6-8 weeks.
In patients with pre-existing anemia, leukopenia and/or thrombocytopenia, as well as in patients with impaired bone marrow function or at risk of developing such disorders, the risk of hematological disorders increases. If this type of phenomenon occurs, a “washing” procedure should be used to reduce the level of A771726 in the blood plasma.
If serious hematological reactions, including pancytopenia, occur, discontinue Arava and any other concomitant drug that suppresses bone marrow hematopoiesis and initiate a washout procedure.
Combined use with other treatments
There is currently no information available regarding the concomitant use of leflunomide with antimalarial drugs used in rheumatology (for example, chloroquine and hydroxychloroquine), intramuscular or oral gold preparations, D-penicillamine, azathioprine and other immunosuppressive drugs (except methotrexate). The risk associated with the prescription of complex therapy, especially with long-term treatment, is unknown. Since this type of therapy can lead to the development of additive or even synergistic toxicity (for example, hepato- or hematotoxicity), combinations of this drug with other basic drugs (for example, methotrexate) are not advisable.
Switching to other types of treatment
Because leflunomide remains in the body for a long time, switching to another disease-modifying drug (eg, methotrexate) without an appropriate washout procedure may increase the potential for additional risks even long after switching (eg, kinetic interactions, organ toxicity).
Likewise, recent treatment with hepatotoxic or haematoxic drugs (eg methotrexate) may lead to an increase in adverse events, so when starting treatment with leflunomide, it is necessary to carefully consider all the positive and negative aspects associated with taking this drug.
Skin reactions
If ulcerative stomatitis develops, leflunomide should be discontinued.
Very rare cases of Stevens-Johnson syndrome or toxic epidermal necrolysis have been reported in patients receiving leflunomide. If skin and/or mucosal reactions occur, you should stop taking Arava and any other related drug and immediately begin a washout procedure. It is necessary to achieve complete elimination of the drug from the body. In such cases, re-prescribing the drug is contraindicated.
Infections
It is known that drugs like leflunomide, which have immunosuppressive properties, make patients more susceptible to various types of infections, including opportunistic infections (infections caused by fungi and microorganisms that can cause infections only in conditions of decreased immunity). Infectious diseases that arise are usually severe and require early and intensive treatment. If a severe infection occurs, it may be necessary to interrupt leflunomide treatment and initiate a washout procedure.
Tuberculin-positive patients should be closely monitored due to the risk of reactivation of tuberculosis.
Respiratory reactions
Rare cases of interstitial pulmonary disease have been reported during leflunomide therapy. Symptoms such as cough and dyspnea may be a reason to stop taking leflunomide.
Blood pressure
Blood pressure levels should be monitored before starting treatment with leflunomide and periodically after starting it.
Interactions
Caution should be exercised when prescribing drugs metabolized by CYP2C9 (phenytoin, warfarin, tolbutamide), with the exception of NSAIDs (non-steroidal anti-inflammatory drugs).
Recommendations for men
There is no data on the risk of fetotoxicity (associated with the toxic effect of the drug on the father’s sperm) when leflunomide is used by men. Experimental data in this direction have not been carried out. To minimize the possible risk, men planning to have a child should stop taking leflunomide and use cholestyramine 8 g 3 times a day for 11 days or 50 g of powdered activated carbon 4 times a day for 11 days.
Active ingredient
Active ingredient
Leflunomide
Composition
Composition
Active substance:
leflunomide 10 mg.
Contraindications
Contraindications
liver dysfunction;
severe immunodeficiency conditions (including AIDS);
severe disorders of bone marrow hematopoiesis or anemia, leukopenia, thrombocytopenia as a result of other causes (except rheumatoid arthritis);
severe infections;
moderate or severe renal failure (due to limited clinical experience);
severe hypoproteinemia (including with nephrotic syndrome);
pregnancy;
lactation (breastfeeding period);
children and adolescents up to 18 years of age;
hypersensitivity to the components of the drug.
Arava is contraindicated in women of childbearing potential who are not using adequate contraception.
Men receiving treatment with leflunomide should be warned about the possible fetotoxic effect of the drug and the need to use adequate contraception.
Side Effects
Side Effects
Classification of the expected frequency of side effects:
very common (more than 1/10), common (more than 1/100, but less than 1/10), infrequent (more than 1/1000, but less than 1/100), rare (more than 1/10,000, but less than 1/1000), very rare (less than 1/10,000), unknown (cannot be estimated based on the available data).
– Cardiovascular system
Common: moderate increase in blood pressure.
Rare: marked increase in blood pressure
– Gastrointestinal tract
Common: diarrhea, nausea, vomiting, diseases of the oral mucosa (for example, aphthous stomatitis, lip ulceration), abdominal pain.
Uncommon: taste disturbances
Very rare: pancreatitis
– Respiratory system and mediastinal disorders
Rare: interstitial pulmonary process (including interstitial pneumonia), possibly fatal.
– Metabolic disorders
Common: increased creatine phosphokinase (CPK)
Uncommon: hypokalemia, hyperlipidemia, hypophosphatemia.
Rare: increased lactate dehydrogenase (LDH) levels
Frequency unknown: hypouricemia
– Nervous system
Frequent: headache, dizziness, paresthesia.
Uncommon: restlessness.
Very rare: peripheral neuropathy
– Musculoskeletal system
Frequent: tenosynovitis.
Uncommon: tendon rupture
– Leather and derivatives
Common: increased hair loss, eczema, rash (including maculopapular rash), itching, dry skin.
Uncommon: urticaria
Very rare: toxic epidermal necrolysis (Lyell’s syndrome), erythema multiforme, Stevens-Johnson syndrome.
– Immune system
Common: mild allergic reactions.
Very rare: serious anaphylactic/anaphylactoid reactions, vasculitis, including cutaneous necrotizing vasculitis.
– Infections and infestations
Rare: development of severe infections, including opportunistic infections, and sepsis, which can be fatal.
The number of possible infections (in particular rhinitis, bronchitis and pneumonia) may increase.
– Hematopoietic and lymphatic system
Common: leukopenia (white blood cells > 2000/µl).
Uncommon: anemia, mild thrombocytopenia (platelets < 100,000/µl).
Rare: pancytopenia (probably due to antiproliferative effects), leukopenia (white blood cells < 2000/μl), eosinophilia.
Very rare: agranulocytosis.
Recent, concomitant, or subsequent use of potentially myelotoxic agents may be associated with a greater risk of hematologic effects.
– Hepato-biliary system
Frequent: increased activity of liver transaminases (especially alanine aminotransferase (ALT)), less often – gamma-glutamyl transpeptidase (GGT) and alkaline phosphatase (ALP), hyperbilirubinemia.
Rare: hepatitis, jaundice/cholestasis.
Very rare: severe liver damage such as liver failure, acute liver necrosis, which can be fatal;
– General changes
Common: anorexia, weight loss (usually minor), asthenia.
– From the reproductive system:
Not known: slight decrease in sperm concentration, total sperm count and motility
– From the kidneys and urinary tract:
Frequency unknown: renal failure
– Other
The risk of malignancy, especially lymphoproliferative diseases, increases with the use of certain immunosuppressive drugs.
Interaction
Interaction
Increased side effects may occur with recent or concomitant use of hepatotoxic (including alcohol) or hematotoxic and immunosuppressive drugs, or when these drugs are started after treatment with leflunomide without a washout procedure (see “Special Instructions”).
In patients with rheumatoid arthritis, no pharmacokinetic interaction was found between leflunomide (10–20 mg per day) and methotrexate (10–25 mg per week).
It is recommended that patients taking leflunomide not be given cholestyramine or activated charcoal as this results in a rapid and significant decrease in plasma concentrations of A771726 (the active metabolite of leflunomide). This is believed to be due to impaired recirculation of A771726 in the liver and small intestine and/or impaired gastrointestinal dialysis.
If the patient is already taking non-steroidal anti-inflammatory drugs (NSAIDs) and/or corticosteroids, they can be continued after starting treatment with leflunomide.
The enzymes involved in the metabolism of leflunomide and its metabolites are not precisely known. An in vivo study of its interaction with cimetidine (a non-specific cytochrome P450 inhibitor) showed no significant interaction. Following concomitant administration of a single dose of leflunomide to subjects receiving multiple doses of rifampicin (a non-specific cytochrome P450 inducer), peak levels of A771726 increased by approximately 40%, whereas the area under the concentration-time curve did not change significantly. The mechanism of this effect is not clear.
In vitro studies have shown that A771726 inhibits the activity of cytochrome P4502C9 (CYP2C9). In clinical trials, no problems were observed with coadministration of leflunomide and NSAIDs metabolized by CYP2C9. Extreme caution should be used when leflunomide is given with other non-NSAID drugs metabolized by CYP2C9 such as phenytoin, warfarin and tolbutamide. An increase in prothrombin time has been reported with the simultaneous administration of leflunomide and warfarin.
In a study in which leflunomide was given to healthy female volunteers concomitantly with triphasic oral contraceptives containing 30 mcg ethinyl estradiol, no decrease in the contraceptive effect of the tablets was observed, and the pharmacokinetics of A771726 were well within the prescribed range.
Currently, there is no information regarding the combined use of leflunomide with antimalarial drugs used in rheumatology (for example, chloroquine and hydroxychlorine), Au preparations (IM or orally), D-penicillamine, azathioprine and other immunosuppressive drugs (with the exception of methotrexate). The risk associated with complex therapy, especially with long-term treatment, is unknown. Since this type of therapy can lead to the development of additive or even synergistic toxicity (for example, hepato- or hematotoxicity), combinations of this drug with other basic drugs (for example, methotrexate) are undesirable. Recent concomitant or subsequent use of potentially myelotoxic agents may be associated with a greater risk of hematologic effects.
Immunosuppressants increase the risk of developing infections, as well as malignancies, especially lymphoproliferative diseases.
Vaccination
There are no clinical data regarding the effectiveness and safety of vaccination in the setting of leflunomide treatment. However, vaccination with live vaccines is not recommended. The long half-life of Arava should be taken into account when planning vaccination with a live vaccine after discontinuation of Arava.
Overdose
Overdose
Symptoms
There have been reports of chronic overdose in patients receiving leflunomide at doses up to 5 times the recommended daily dose, as well as reports of acute overdose in adults and children. In most cases of overdose, no adverse events were reported. Occurring adverse events were comparable to the safety profile of leflunomide. The most commonly observed adverse events were diarrhea, abdominal pain, leukopenia, anemia, and increased liver function tests.
Treatment
In case of overdose or toxicity, it is recommended to take cholestyramine or activated carbon to speed up the cleansing of the body.
Cholestyramine administered orally at 8 g three times daily for 24 hours to three healthy volunteers reduced plasma levels of A771726 by approximately 40% after 24 hours and by 49 to 65% after 48 hours.
It was shown that the administration of activated carbon (powder made into a suspension) orally or by gastric tube (50 g every 6 hours for 24 hours) reduced the concentration of the active metabolite A771726 in plasma by 37% after 24 hours and by 48% after 48 hours.
These “washing” procedures can be repeated according to clinical indications.
Studies with hemodialysis and CAPD (chronic ambulatory peritoneal dialysis) indicate that A771726, the main metabolite of leflunomide, is not excreted by dialysis.
Storage conditions
Storage conditions
At a temperature not exceeding 25 °C
Shelf life
Shelf life
3 years
Manufacturer
Manufacturer
Opella Healthcare International CAC, France
Additional information
| Shelf life | 3 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 °C |
| Manufacturer | Opella Healthcare International SAS, France |
| Medication form | pills |
| Brand | Opella Healthcare International SAS |
Related products
Buy Arava, 10 mg 30 pcs. with delivery to USA, UK, Europe and over 120 other countries.