No products in the cart.
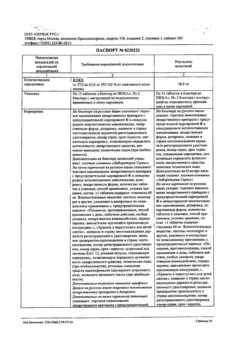
Apidra SoloStar, 100 units/ml 3 ml cartridges in syringe pens 5 pcs
€59.34 €49.45
Description
Hypoglycemic drug. Insulin glulisine is a recombinant analog of human insulin, which is equivalent in action to regular human insulin.
The action of glulisine insulin is faster and shorter in duration than standard human insulin. The mechanism of action of glulisine insulin is regulation of glucose metabolism.
Insulin preparations lower blood glucose levels by stimulating peripheral glucose consumption, especially by skeletal muscle and adipose tissue, and by inhibiting glucose production by the liver.
Insulin suppresses lipolysis in adipocytes, inhibits proteolysis and stimulates protein synthesis. When administered by injection glulisine action starts significantly earlier and lasts shorter compared to human insulin preparations: its hypoglycemic activity starts after 10-20 minutes.
Hypoglycemic effects of insulin glulisine and human insulin are equivalent when given by injection. One unit of glulisine insulin has the same hypoglycemic effect as one unit of human insulin.
Indications
Indications
The treatment of diabetes in adults, adolescents and children 6 years and older when insulin therapy is needed.
Active ingredient
Active ingredient
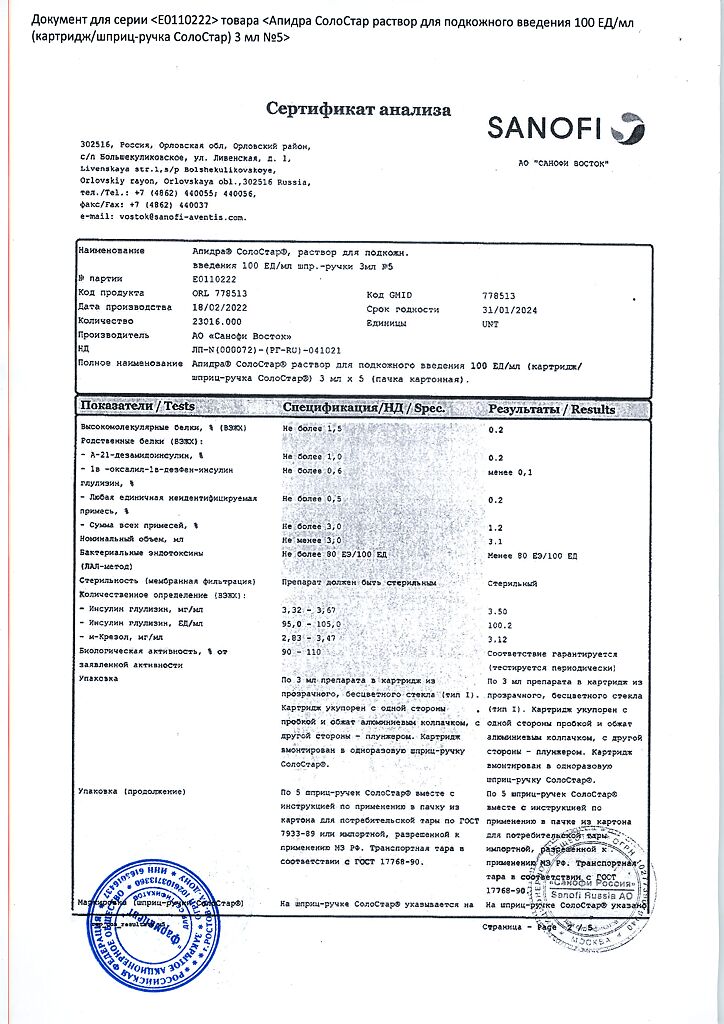
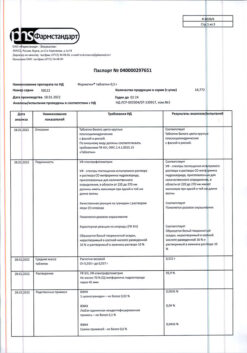
Composition
Composition
1 ml contains insulin glulisine 100 IU (3.49 mg);
auxiliary substances:
methacresol (m-cresol),
trometamol,
sodium chloride,
polysorbate 20,
sodium hydroxide,
hydrochloric acid,
water d / i.
How to take, the dosage
How to take, the dosage
Ã/q, shortly (0-15 minutes) before or shortly after a meal.
Apidra SoloStar should be used in treatment regimens that include either medium-acting insulin or long-acting insulin or a long-acting insulin analog.
In addition, the drug Apidra SoloStar can be used in combination with oral hypoglycemic agents.
The dosing regimen of Apidra SoloStar is chosen individually.
Interaction
Interaction
There have been no studies on pharmacokinetic interactions. Based on the available empirical knowledge with respect to other similar drugs, the occurrence of clinically significant pharmacokinetic interactions is unlikely.
Some substances may affect glucose metabolism, which may require adjustment of glulisine insulin doses and particularly close monitoring of treatment. Substances that can increase the hypoglycemic effect of insulin and increase the susceptibility to hypoglycemia include: oral hypoglycemic agents, angiotensin-converting enzyme inhibitors, disopyramide, fibrates, fluoxetine, monoamine oxidase inhibitors, pentoxifylline, propoxifen, salicylates and sulfonamide antimicrobials. Substances that can reduce the hypoglycemic effects of insulin include: GCSs, danazol, diazoxide, diuretics, isoniazid, phenothiazine derivatives, somatropin, sympathomimetics (e.g. epinephrine (adrenaline), salbutamol, terbutaline), thyroid hormones, estrogens, progestins (for example in oral contraceptives), protease inhibitors and antipsychotic medications (for example olanzapine and clozapine).
Special Instructions
Special Instructions
The patient must be switched to a new type of insulin or insulin from another manufacturer under close medical supervision, as a change in dose may be necessary due to changes in insulin concentration, brand (manufacturer), type of insulin (soluble, isophane, etc.), type of insulin (animal origin) and/or production method.
In addition, correction of concomitant oral hypoglycemic therapy may be required.
The use of inadequate doses of insulin or discontinuation of treatment, especially in patients with type 1 diabetes, may lead to the development of hyperglycemia and diabetic ketoacidosis, conditions that are potentially life-threatening.
Contraindications
Contraindications
Hypersensitivity to insulin glulisine or to any of the drug components; Hypoglycemia.
Pregnant women should use with caution.
Side effects
Side effects
Hypoglycemia is the most common adverse effect of insulin therapy, which can occur if too high doses of insulin are used in excess of the need for it.
The adverse reactions associated with the drug administration observed in clinical trials are listed below by organ system and in decreasing order of occurrence. The following criteria are used to describe the frequency of occurrence: very common, > 10%; common, > 1% and < 10%; sometimes, > 0.1% and < 1%; rare, > 0.01% and < 0.1%; very rare, < 0.01%.
Metabolic disorders: very often – hypoglycemia. Symptoms of hypoglycemia usually occur suddenly. However, usually neuropsychiatric disorders against the background of neuroglycopenia (feeling of fatigue, unusual fatigue or weakness, reduced ability to concentrate, drowsiness, visual disturbances, headache, nausea, confusion or loss of consciousness, seizure syndrome) are preceded by symptoms of adrenergic counter-regulation (sympathoadrenal system activation in response to hypoglycemia): feeling of hunger, irritability, nervous excitement or tremor, anxiety, pale skin, “cold” sweat, tachycardia, pronounced palpitations (the faster hypoglycemia develops and the more severe it is, the more pronounced are the symptoms of adrenergic counterregulation).
Episodes of severe hypoglycemia, especially repeated, may lead to damage of the nervous system. Episodes of prolonged and severe hypoglycemia may be life-threatening for patients, as even fatal outcome is possible if hypoglycemia increases.
Local reactions: often – local reactions of hypersensitivity (hyperemia, swelling and itching at the injection site). These reactions are usually transient and disappear with continuation of treatment; rarely – lipodystrophy (as a result of violation of the alternation of places of injection of insulin in any of the areas /insertion of the drug in the same place/).
Allergic reactions: sometimes – hives, tightness in the chest, bronchospasm, allergic dermatitis, itching. Severe cases of generalized allergic reactions (including anaphylactic) can be life-threatening.
Overdose
Overdose
Symptoms:There are no specific data on glulisine insulin overdose; hypoglycemia of varying severity may develop.
Treatment: episodes of mild hypoglycemia can be managed with glucose or sugar-containing products. Therefore, it is recommended that diabetic patients have sugar cubes, candy, cookies, or sweet fruit juice with them at all times.
Episodes of severe hypoglycemia, during which the patient loses consciousness, may be controlled by an injection of 0.5-1 mg of glucagon or by an intravenous injection of dextrose (glucose). If the patient does not respond to glucagon administration within 10-15 minutes, dextrose should also be administered intravenously.
After recovery of consciousness, it is recommended to give the patient oral carbohydrates to prevent recurrence of hypoglycemia. After glucagon administration to determine the cause of this severe hypoglycemia and to prevent the development of other similar episodes, the patient should be monitored in the hospital.
Pregnancy use
Pregnancy use
There is insufficient information on the use of insulin glulisine in pregnant women.
Animal reproductive studies have shown no differences between insulin glulisine and human insulin with respect to pregnancy course, fetal/fetal development, labor and postnatal development.
Apidra SoloStar should be used with caution in pregnant women. Close monitoring of blood glucose levels is mandatory. Patients with pre-existing or gestational diabetes mellitus should maintain optimal metabolic control throughout pregnancy.
The need for insulin may decrease during the first trimester of pregnancy, and may generally increase during the second and third trimesters. Immediately after delivery, the need for insulin decreases rapidly. Nursing mothers may need to adjust their insulin doses and diet.
Additional information
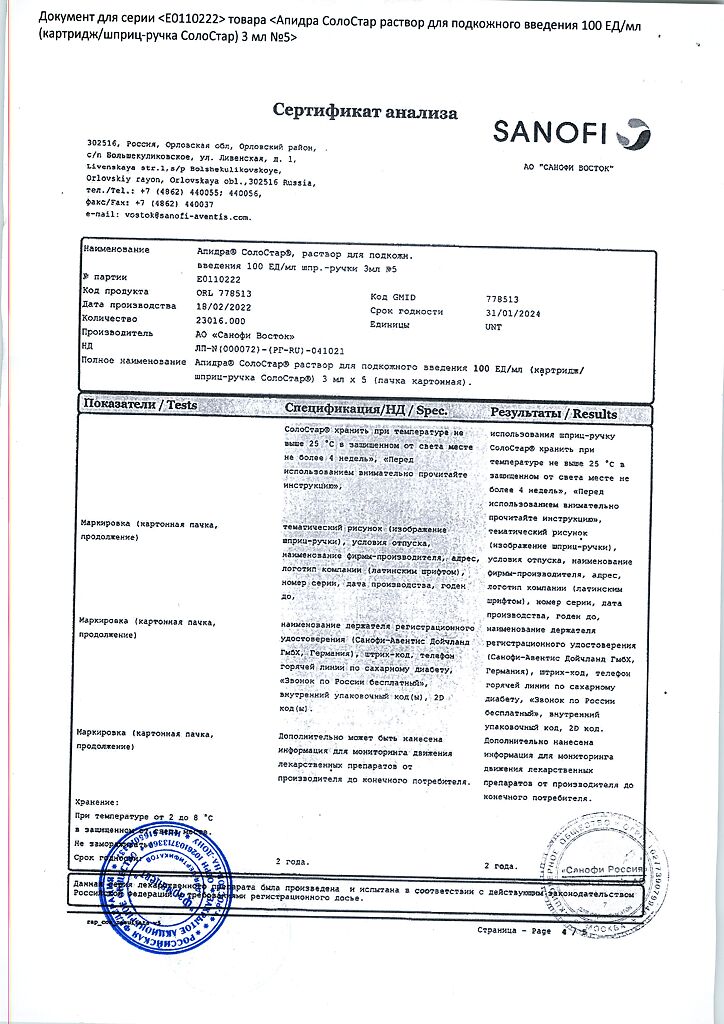
| Weight | 0.169 kg |
|---|---|
| Shelf life | 2 years |
| Conditions of storage | In the dark place at 2-8 °C (do not freeze) |
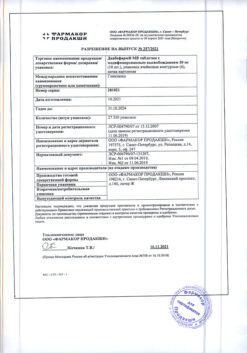
| Manufacturer | Sanofi-Vostok JSC, Russia |
| Medication form | solution |
| Brand | Sanofi-Vostok JSC |
Related products
Buy Apidra SoloStar, 100 units/ml 3 ml cartridges in syringe pens 5 pcs with delivery to USA, UK, Europe and over 120 other countries.