No products in the cart.
Amprilan ND, tablets 5 mg+25 mg 30 pcs
€20.02 €16.69
Description
Ramipril.
A ACE inhibitor, prevents conversion of angiotensin I to angiotensin II without a compensatory increase in heart rate. It reduces the production of aldosterone, OPPS, pulmonary capillary pressure, pulmonary vascular resistance, does not change glomerular filtration rate, and increases coronary blood flow. Long-term use of the drug decreases myocardial hypertrophy in patients with arterial hypertension, reduces the rate of myocardial reperfusion arrhythmias, improves blood flow to the ischemic myocardium. The cardioprotective effect is due to the influence on PG synthesis and induction of nitric oxide formation in endotheliocytes. The drug reduces platelet aggregation. The onset of hypotensive action is 1.5 h after oral administration, the maximum effect is in 5-9 h, the duration of action is 24 h. Ramipril does not cause withdrawal syndrome.
Hydrochlorothiazide.
Thiazide diuretic, its diuretic effect is associated with disruption of reabsorption of sodium, chloride, potassium, magnesium and water ions in the distal nephron; it delays excretion of calcium and uric acid ions. It has antihypertensive properties. It has practically no effect on normal BP. Diuretic effect occurs after 1-2 hours, reaches a maximum after 4 hours and lasts for 6-12 hours. Antihypertensive effect occurs within 3-4 days, but it may take 3-4 weeks to achieve optimal therapeutic effect. Ramipril and hydrochlorothiazide have additive effects. Ramipril reduces the loss of potassium ions caused by taking hydrochlorothiazide.
Indications
Indications
Arterial hypertension (patients who are indicated for combination therapy).
Active ingredient
Active ingredient
Composition
Composition
Active substances:
Ramipril – 5 mg,
Hydrochlorothiazide – 25 mg.
Auxiliary substances:
Sodium bicarbonate;
Lactose monohydrate;
croscarmellose sodium;
Pregelatinized starch (starch 1500);
sodium stearyl fumarate.
How to take, the dosage
How to take, the dosage
Internally. The dose is adjusted individually. Daily dose for adults is 1 tablet per day.
In mild to moderate renal dysfunction (creatinine Cl > 30 ml/min, serum creatinine is approximately 3 mg/dL or 265 µmol/L), the usual dose of the drug is recommended. In Cl creatinine
The duration of therapy is not limited.
Interaction
Interaction
Ramipril.
It enhances the CNS depressant effect of ethanol.
Ingestion of salt with food may decrease the hypotensive effect of ramipril.
The concomitant use of ramipril and other drugs that reduce BP (e.g., diuretics, nitrates, tricyclic antidepressants, drugs for general anesthesia) leads to increased hypotensive effect of ramipril. Concomitant administration of ramipril and potassium preparations or potassium-saving diuretics may cause hyperkalemia.
Vasopressor sympathomimetics (epinephrine, norepinephrine) may decrease the hypotensive effect of ramipril. Therefore, BP levels should be carefully monitored during concomitant treatment.
The concomitant administration of ramipril and allopurinol, immunosuppressants, corticosteroids, procainamide, cytostatics increases the possibility of peripheral blood count changes (risk of leukopenia).
The concomitant administration of ramipril and lithium drugs leads to decreased excretion of lithium, therefore serum lithium concentration should be monitored – risk of toxic effects.
The ACE inhibitors may increase the effect of hypoglycemic agents (e.g., insulin or sulfonylurea derivatives), which in some cases may cause hypoglycemia. In this regard, blood sugar levels should be monitored carefully, especially at the beginning of concomitant use.
The concomitant use of ramipril and NSAIDs (e.g., acetylsalicylic acid and indomethacin) may impair the hypotensive effect of ramipril.
In addition, concomitant use may cause hyperkalemia and increase the risk of renal dysfunction.
The concomitant use of ramipril with estrogens may weaken the hypotensive effect.
The concomitant use of heparin and ramipril may cause hyperkalemia.
Anaphylactic and anaphylactoid reactions to stinging insect venom (and possibly to other allergens) are more severe during treatment with ACE inhibitors.
Hydrochlorothiazide.
The simultaneous use of foxglove glycosides with thiazide diuretics increases the possibility of toxic effects of the glycosides (including increased ventricular excitability) due to the likely development of hypokalemia and hypomagnesemia.
The drugs that intensively bind to blood proteins (indirect anticoagulants, clofibrate, NSAIDs) increase the diuretic effect of hydrochlorothiazide.
The hypotensive effect of hydrochlorothiazide is enhanced by vasodilators, beta-adrenoblockers, barbiturates, phenothiazines, tricyclic antidepressants, ethanol.
Hydrochlorothiazide increases neurotoxicity of salicylates, reduces the effect of oral hypoglycemic agents, norepinephrine, epinephrine and antipodagric agents, increases cardiotoxic and neurotoxic effects of lithium drugs, effects of peripheral muscle relaxants, reduces excretion of quinidine.
The simultaneous use of methyldopa may lead to hemolysis.
Colestyramine decreases absorption of hydrochlorothiazide.
Hydrochlorothiazide reduces the effect of oral contraceptives.
Special Instructions
Special Instructions
Ramipril.
Renal function should be assessed at the start of treatment. Renal function should be carefully monitored during treatment with ramipril especially in patients with impaired renal function, with renal vascular disease (e.g. clinically insignificant renal artery stenosis or hemodynamically significant artery stenosis of the sole kidney); heart failure.
The risk of hypersensitivity and allergy-like (anaphylactoid) reactions is increased in patients concomitantly receiving ACE inhibitors and undergoing hemodialysis procedures using AN69 dialysis membranes. Similar reactions have been found with low-density lipoprotein apheresis using dextran sulfate, so this method should be avoided during treatment with ACE inhibitors.
During treatment with ramipril, serum urea and creatinine levels may increase in patients with impaired renal function, especially with concomitant treatment with diuretics. In this case, treatment should be continued with lower doses of ramipril or the drug should be discontinued. In patients with impaired renal function the risk of hyperkalemia increases.
In patients with impaired hepatic function due to decreased activity of “hepatic” enzymes the metabolism of ramipril and formation of active metabolite may be delayed. In this regard, treatment of such patients should be started only under close medical supervision.
Patients on low-salt or no-salt diet should be used with caution when administering ramipril (increased risk of arterial hypotension) In patients with decreased blood circulation (as a result of diuretic therapy), during dialysis, in diarrhea and vomiting symptomatic hypotension may develop.
Transient arterial hypotension is not a contraindication to continue treatment after BP stabilization. In case of recurrence of severe arterial hypotension, the dose should be reduced or the drug should be discontinued. In patients undergoing extensive surgery or receiving other agents causing arterial hypotension during general anesthesia, ramipril may cause angiotensin II blockade with compensatory renin release. If the physician associates the development of arterial hypotension with the above mechanism, the arterial hypotension may be corrected by increasing the blood plasma volume.
In rare cases during treatment with ACE inhibitors agranulocytosis, erythrocytopenia, thrombocytopenia, hemoglobinemia or bone marrow depression have been observed. At the beginning and during treatment, it is necessary to monitor the number of white blood cells to detect possible neutropenia/agranulocytosis. More frequent monitoring is recommended in patients with renal insufficiency, with connective tissue diseases (e.g., systemic lupus erythematosus or scleroderma) and in patients simultaneously taking drugs that affect hematopoiesis (see “Interactions”). Count of blood cells should also be performed in case of clinical signs of neutropenia/agranulocytosis and increased bleeding.
In patients with arterial hypertension during treatment with ramipril an increase in serum potassium levels is rarely observed. The risk of hyperkalemia is increased in chronic heart failure, concomitant treatment with potassium-saving diuretics (spironolactone, amiloride, triamterene) and administration of potassium preparations.
When ACE inhibitors are used during desensitization therapy to aspen or bee venom, anaphylactoid reactions (such as arterial hypotension, dyspnea, vomiting, skin rash) may occur, which can be life-threatening. Hypersensitivity reactions can occur with insect stings (e.g. bee or wasp stings). If desensitizing treatment with bee or wasp venom is necessary, ACE inhibitors should be stopped and treatment should be continued with suitable drugs from other groups.
Hydrochlorothiazide.
To prevent potassium and magnesium deficiency, a diet high in potassium and magnesium, potassium-saving diuretics, and potassium and magnesium salts are prescribed. Regular monitoring of plasma levels of potassium, glucose, uric acid, lipids, and creatinine is necessary.
Impact on the ability to drive and operate machinery.
During treatment, caution should be exercised when driving motor vehicles, as well as during potentially hazardous activities requiring increased concentration and rapid psychomotor reactions.
Contraindications
Contraindications
Ramipril.
With caution: severe lesions of coronary and cerebral arteries (risk of decreased blood flow with excessive BP reduction); unstable angina pectoris; severe ventricular rhythm disorders; chronic heart failure stage IV; decompensated “pulmonary heart”; renal and/or liver failure; hyperkalemia, hyponatremia (incl.Ñ. against the background of diuretics and diet with salt restriction); conditions accompanied by the decrease of the blood circulation (including diarrhea, vomiting); systemic connective tissue diseases, including scleroderma and systemic lupus erythematosus; diseases requiring prescription of GCS and immunosuppressants (no clinical experience); diabetes; suppression of bone marrow hematopoiesis; old age.
Hydrochlorothiazide.
With caution: hypokalemia, hyponatremia, hypercalcemia; CHD; liver failure, cirrhosis; history of bronchial asthma; advanced age.
Side effects
Side effects
Ramipril.
Cardiovascular system disorders: decreased BP, orthostatic hypotension, orthostatic collapse, tachycardia, rarely – arrhythmia, palpitation, exacerbation of Raynaud’s syndrome. In excessive BP reduction, mainly in patients with CHD and clinically significant cerebral vasoconstriction, myocardial ischemia (myocardial infarction angina) and cerebral ischemia (possibly with dynamic cerebral circulation disorder or stroke) may develop.
Urogenital system disorders: development or worsening of symptoms of renal failure, proteinuria, oliguria, interstitial nephritis, nephrotic syndrome, decreased urine volume, gynecomastia, decreased potency, libido.
CNS disorders: dizziness, headache, weakness, somnolence, peripheral neuropathy (paresthesias), nervous excitability, anxiety, tremor, muscle spasm, mood disorders, apathy; in high doses – insomnia, anxiety, depression, ataxia, confusion, fainting.
Sensory organs: vestibular disorders, disorders of taste (e.g. metallic taste), smell, hearing and vision, blepharitis, dry conjunctivae, lacrimation, tinnitus.
Digestive system disorders: Nausea, vomiting, diarrhea or constipation, pain in the epigastric region, intestinal obstruction, flatulence, pancreatitis, hepatitis, cholestatic jaundice, cholecystitis (in the presence of cholelithiasis), liver function disorder with development of liver failure, melena, ileus, dry mouth, thirst, reduced appetite, stomatitis, glossitis, inflamed salivary glands.
Respiratory system: “dry” cough, bronchospasm, dyspnea, rhinorrhea, rhinitis, sinusitis, pharyngitis, hoarseness, bronchitis, interstitial pneumonia, pulmonary embolism, pulmonary infarction, pulmonary edema.
Allergic reactions: skin rash, pruritus, urticaria, conjunctivitis, photosensitization, angioedema of the face, extremities, lips, tongue, pharynx and/or larynx, exfoliative dermatitis, erythema multiforme (including Stevens-Jung’s syndrome).Stevens-Johnson syndrome), toxic epidermal necrolysis (Lyell’s syndrome), vesicles, serositis, onycholysis, vasculitis, myositis, muscle weakness, myalgia, arthralgia, arthritis, eosinophilia.
Others: seizures, alopecia, shingles, hyperthermia, increased sweating. Laboratory indexes: hypercreatininemia, increased urea nitrogen level, increased “liver” enzymes activity, hyperbilirubinemia, hyperkalemia, hyponatremia, anemia, decrease of hemoglobin concentration and hematocrit, neutropenia, thrombocytopenia, agranulocytosis, pancytopenia, hemolytic anemia, appearance of antinuclear antibodies.
Fetal effects: impaired fetal function, decreased fetal and neonatal BP, impaired renal function, hyperkalemia, skull bone hypoplasia, oligohydramnios, limb contracture, skull bone deformity, lung hypoplasia.
Hydrochlorothiazide.
Water-electrolyte and acid-base balance: possible development of hypokalemia and hypochloremic alkalosis (dry mouth, increased thirst, heart rhythm disturbances, mood and mental changes, cramps or muscle pain, nausea, vomiting, weakness; hypochloremic alkalosis may lead to hepatic encephalopathy or hepatic coma), hyponatremia (confusion, convulsions, apathy, slowed thinking process, fatigue, irritability), hypomagnesemia (arrhythmias).
Hematopoietic system disorders: agranulocytosis, thrombocytopenia, hemolytic and aplastic anemia, leukocytopenia, eosinophilia, neutropenia, pancytopenia.
Cardiovascular system: arrhythmia, orthostatic hypotension, tachycardia.
Digestive system disorders: cholecystitis, pancreatitis, jaundice, diarrhea, sialadenitis, constipation, anorexia, epigastric pain.
Metabolism disorders: hypercholesterolemia, hypertriglyceridemia, hyperglycemia, glucosuria, hyperuricemia, hypercalcemia, worsening of gout.
CNS disorders: depression, sleep disturbance, anxiety, paresthesias, confusion, dizziness.
Sensory organs: xanthopsia, visual disturbances.
Urinary system disorders: impaired renal function, decreased potency, interstitial nephritis.
Allergic reactions: skin rash, urticaria, purpura, necrotizing vasculitis, Stevens-Johnson syndrome, respiratory distress syndrome (pneumonitis, noncardiac pulmonary edema), toxic epidermal necrolysis, photosensitization; anaphylactic reactions (up to life-threatening anaphylactic shock).
Others: hyperthermia, weakness.
Overdose
Overdose
Ramipril.
Symptoms: marked BP decrease, bradycardia, shock, disruption of water-electrolyte balance, acute renal failure, stupor, dry mouth, weakness, somnolence.
Treatment: the patient should be in horizontal position with elevated legs, in mild cases of overdose – gastric lavage, administration of adsorbents and sodium sulfate (preferably within the first 30 minutes after taking the drug). If BP decreases – intravenous administration of catecholamines, angiotensin II; if bradycardia – use pacing agent. The drug is not excreted during hemodialysis.
Hydrochlorothiazide.
Symptoms: hypokalemia (adynamia, paralysis, constipation, arrhythmias), drowsiness, decreased BP.
Treatment: infusion of electrolyte solutions; compensation for K+ deficiency (administration of potassium preparations and potassium-saving diuretics).
Pregnancy use
Pregnancy use
It is contraindicated in pregnancy and lactation.
Similarities
Similarities
Additional information
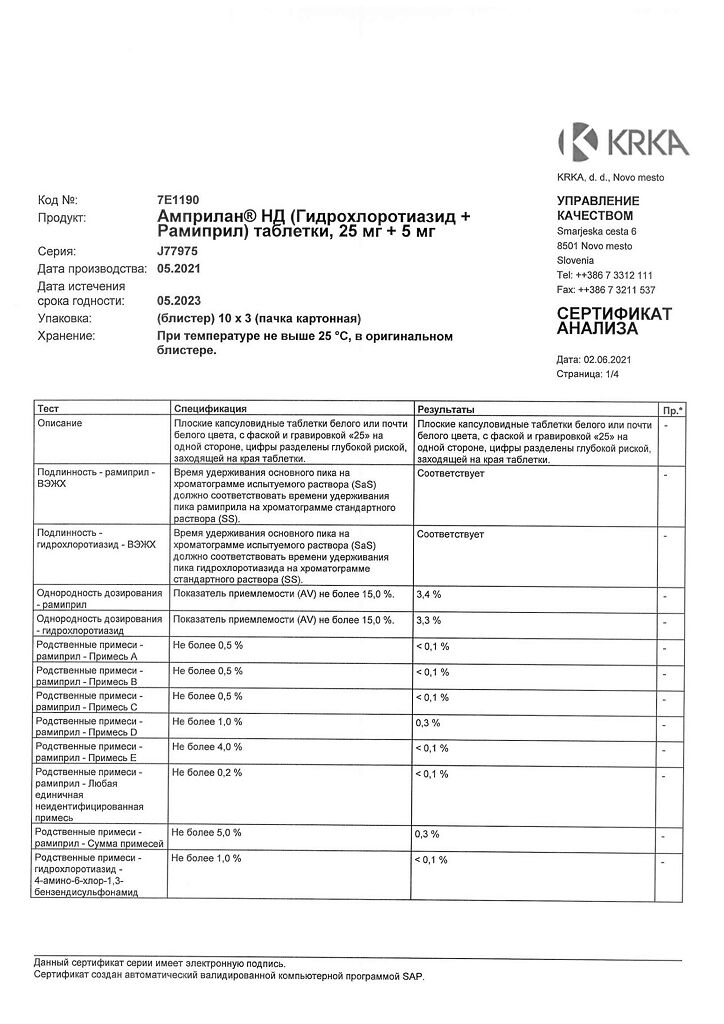
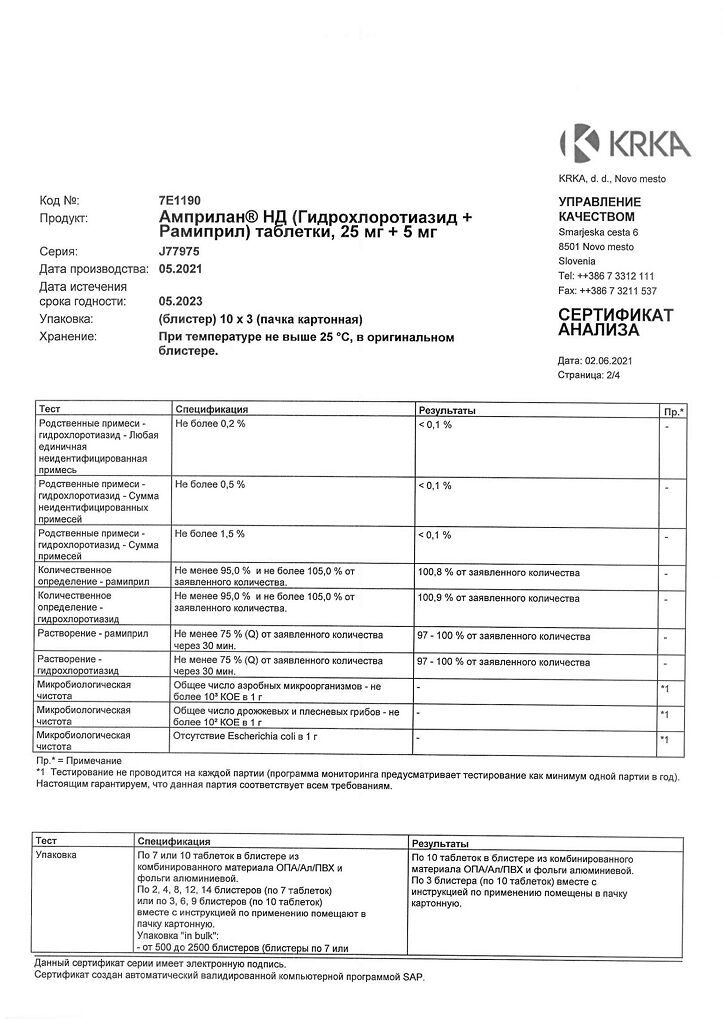
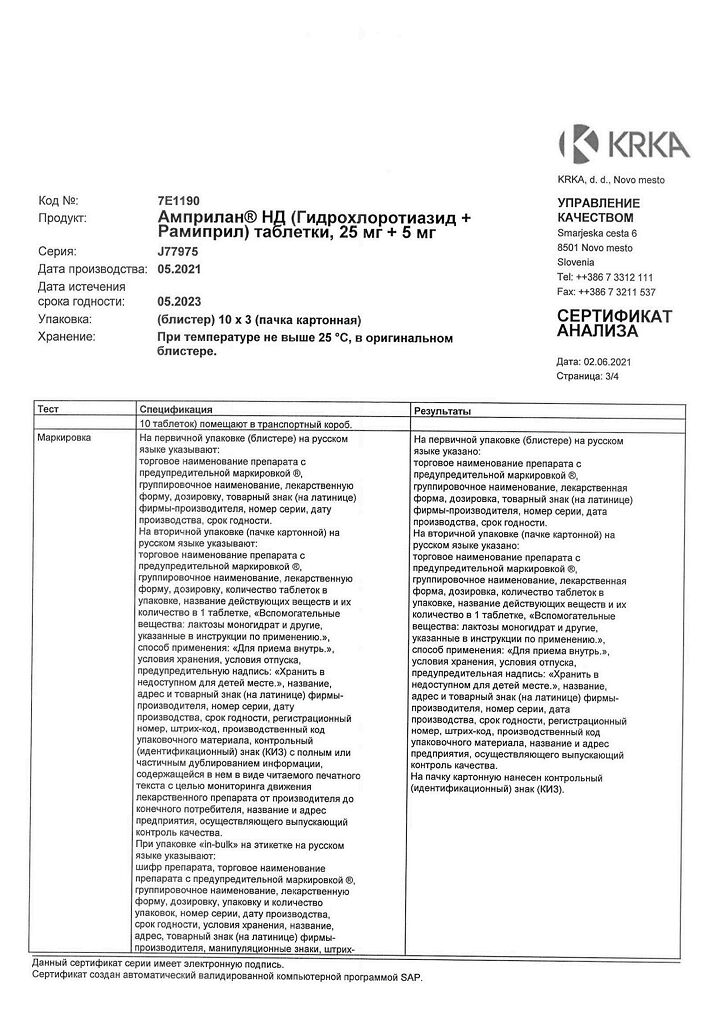
| Weight | 0.024 kg |
|---|---|
| Shelf life | 2 years |
| Conditions of storage | At a temperature not exceeding 25 °C |
| Manufacturer | KRKA dd Novo mesto, Slovenia |
| Medication form | pills |
| Brand | KRKA dd Novo mesto |
Related products
Buy Amprilan ND, tablets 5 mg+25 mg 30 pcs with delivery to USA, UK, Europe and over 120 other countries.