No products in the cart.
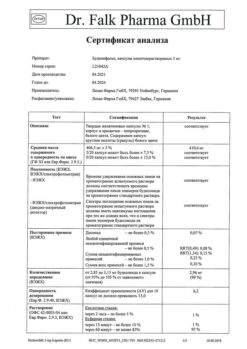
Almont, 10 mg 28 pcs.
€33.72 €28.10
Description
Pharmacotherapeutic group: Anti-inflammatory antibronchoconstrictor agent – leukotriene receptor blocker
ATCode: R03DC03
Pharmacological properties.
Indications
Indications
Prevention and long-term treatment of bronchial asthma in adults and children over 15 years of age, including prevention of daytime and nighttime symptoms of the disease, treatment of bronchial asthma in patients with hypersensitivity to acetylsalicylic acid and prevention of bronchospasm caused by physical activity.
Relief of daytime and nighttime symptoms of seasonal and/or year-round allergic rhinitis in adults and children over 15 years of age.
Pharmacological effect
Pharmacological effect
Pharmacotherapeutic group: anti-inflammatory antibronchoconstrictor agent – leukotriene receptor blocker
ATX code: R03DC03
Pharmacological properties
Special instructions
Special instructions
The effectiveness of the drug Almont for oral administration in the treatment of acute attacks of bronchial asthma has not been established, therefore the drug Almont in tablets is not recommended for the treatment of acute attacks of bronchial asthma. Patients should be instructed to always carry emergency medications to relieve asthma attacks (short-acting inhaled beta2-agonists).
You should not stop taking Almont during an exacerbation of bronchial asthma and the need to use emergency medications to relieve attacks (short-acting inhaled beta2-agonists).
Patients with a confirmed allergy to acetylsalicylic acid and other non-steroidal anti-inflammatory drugs (NSAIDs) should not take these drugs during treatment with Almont, since Almont, while improving respiratory function in patients with allergic bronchial asthma, nevertheless cannot completely prevent bronchoconstriction caused by NSAIDs. The dose of inhaled glucocorticosteroids used simultaneously with the drug Almont can be gradually reduced under the supervision of a physician, however, an abrupt replacement of inhaled or oral glucocorticosteroids with Almont should not be carried out. Neuropsychiatric disorders have been described in patients taking montelukast. Given that these symptoms could be caused by other factors, it is unknown whether they are related to taking Almont. The physician should discuss these AEs with patients and/or their parents/guardians. Patients and/or their parents/guardians should be advised that if such symptoms occur, they should notify their physician. In rare cases, patients receiving anti-asthma drugs, including leukotriene receptor antagonists, have experienced one or more AEs: eosinophilia, skin rash, worsening of pulmonary symptoms, cardiac complications and/or neuropathy, sometimes diagnosed as Churg-Strauss syndrome, systemic eosinophilic vasculitis. These cases were sometimes associated with dose reduction or discontinuation of oral corticosteroid therapy. Although a causal relationship between these AEs and leukotriene receptor antagonist therapy has not been established, caution should be exercised in patients taking Almont; In such patients, appropriate clinical monitoring should be carried out.
Almont contains lactose monohydrate. Patients with a rare form of hereditary galactose intolerance, congenital lactase deficiency or glucose-galactose malabsorption should not take Almont.
Use in elderly patients
There were no differences in the efficacy and safety profiles of montelukast associated with patient age.
Impact on the ability to drive vehicles and machinery
Taking montelukast is not expected to affect the ability to drive vehicles or operate machinery. However, individual reactions to the drug may vary. Some side effects (such as dizziness and drowsiness), which have been reported to occur very rarely with montelukast, may affect the ability of some patients to drive and operate machines. If the described adverse events occur, you should refrain from performing these activities.
Active ingredient
Active ingredient
Montelukast
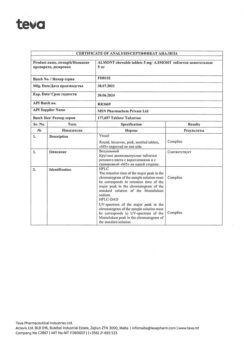
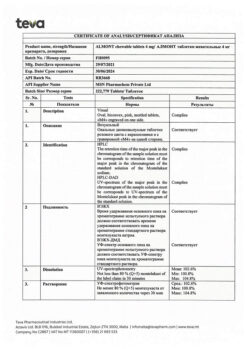
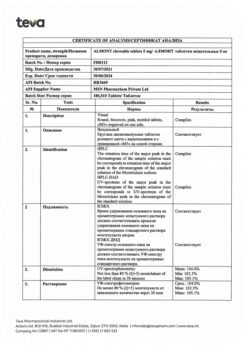
Composition
Composition
1 tablet contains:
Active ingredient
Montelukast (as montelukast sodium)
10.00 mg
(10.40 mg)
Excipients
core
Microcrystalline cellulose, type 102
89.30 mg
Hyprolose
4.00 mg
Croscarmellose sodium
6.00 mg
Lactose monohydrate
89.30 mg
Magnesium stearate
1.00 mg
Core mass
200.00 mg
film casing
Opadry II Beige 31F27012:
Lactose monohydrate
Hypromellose 15cP
Titanium dioxide
Macrogol 4000
Iron oxide yellow dye
Iron oxide red dye
4.0 mg
1,440 mg
1.120 mg
1.011 mg
0.400 mg
0.026 mg
0.003 mg
Total tablet weight
204.00 mg
Pregnancy
Pregnancy
There have been no clinical studies of montelukast in pregnant women. Almont should be used during pregnancy and lactation only if the expected benefit to the mother outweighs the potential risk to the fetus or child. During post-marketing use of montelukast, the development of congenital limb defects has been reported in newborns whose mothers took montelukast during pregnancy. Most of these women also took other medications to treat asthma during pregnancy. A cause-and-effect relationship between taking montelukast and the development of congenital limb defects has not been established.
It is not known whether montelukast is excreted in breast milk. Since many drugs are excreted in breast milk, this must be taken into account when prescribing Almont to breastfeeding mothers.
Contraindications
Contraindications
– hypersensitivity to the active or any excipient of the drug;
– children under 15 years of age;
– lactase deficiency, lactose intolerance, glucose-galactose malabsorption.
Side Effects
Side Effects
In general, montelukast was well tolerated. Side effects are usually mild and, as a rule, do not require discontinuation of the drug. The overall incidence of side effects when treated with the drug is comparable to their frequency when taking placebo.
Adults and children aged 15 years and older with asthma
In two similarly designed, 12-week placebo-controlled clinical trials, the only adverse events (AEs) assessed as drug-related occurring in >1% of montelukast-treated patients and more frequently than in placebo-treated patients were abdominal pain and headache. The differences in the incidence of these AEs between the two treatment groups were not statistically significant. With longer treatment (for 2 years), the AE profile did not change.
Adults and children aged 15 years and older with seasonal allergic rhinitis
Montelukast was taken by patients once daily in the morning or evening and was generally well tolerated, with a safety profile similar to that of placebo. In placebo-controlled clinical trials, there were no AEs considered drug-related that occurred in >1% of patients treated with montelukast or more frequently than in patients treated with placebo. In the 4-week placebo-controlled clinical study, the safety profile of the drug was similar to that in the 2-week studies. The incidence of drowsiness with the drug in all studies was the same as with placebo.
Adults and children aged 15 years and older with year-round allergic rhinitis
Montelukast was taken by patients once daily and was generally well tolerated. The drug’s safety profile was similar to that observed in patients with seasonal allergic rhinitis and placebo. In these clinical studies, there were no AEs that were considered drug-related, occurred in > 1% of patients treated with montelukast, or occurred more frequently than in patients treated with placebo. The incidence of drowsiness while taking the drug was the same as when taking placebo.
Generalized analysis of clinical trial results
A pooled analysis of 41 placebo-controlled clinical trials (35 studies involving patients aged 15 years or older) using validated suicidality assessment tools was conducted. Among the 9,929 patients receiving montelukast and the 7,780 patients receiving placebo in these studies, one patient was identified as suicidal in the montelukast group. There were no suicides, suicide attempts, or other preparatory acts indicative of suicidal behavior in any of the treatment groups.
Separately, a pooled analysis of 46 placebo-controlled clinical trials (35 studies in patients aged 15 years or older and 11 studies in patients aged 3 months to 14 years) was conducted to assess adverse behavioral effects (AEs). Among the 11,673 patients receiving montelukast and 8,827 patients receiving placebo in these studies, the percentage of patients experiencing at least one AE was 2.73% among those receiving montelukast and 2.27% among those receiving placebo: an odds ratio of 1.12 (95% confidence interval [0.93, 1.361]).
The most common side effects associated with the use of the drug were headache and abdominal pain (common).
The incidence of adverse events is assessed according to the following: very common (≥1/10), common (≥1/100 to <1/10), uncommon (≥1/1000 to <1/100), rare (≥1/10,000 to <1/1000), very rare (<1/10,000), unknown (cannot be estimated from the available data).
During post-registration use of the drug montelukast, the following identified adverse reactions were reported:
Infectious and parasitic diseases:
Very common: upper respiratory tract infections.
Blood and lymphatic system disorders:
Rarely: increased tendency to bleed.
Very rare: thrombocytopenia.
Immune system disorders:
Uncommon: hypersensitivity reactions, including anaphylaxis.
Very rare: eosinophilic infiltration of the liver.
Mental disorders:
Uncommon: sleep disturbances, including nightmares, insomnia, somnambulism, irritability, restlessness, agitation, including aggressive behavior or hostility, depression.
Very rare: Hallucinations, disorientation, suicidal thinking and behavior (suicidality), dysphemia.
Nervous system disorders:
Uncommon: dizziness, drowsiness, paresthesia/hypoesthesia, convulsions.
Cardiac disorders:
Rarely: increased heart rate.
Disorders of the respiratory system, chest and mediastinal organs:
Uncommon: nosebleeds.
Very rare: pulmonary eosinophilia.
Gastrointestinal disorders:
Common: diarrhea, nausea, vomiting.
Uncommon: dry mouth, dyspepsia.
Disorders of the liver and biliary tract:
Often: increased activity of alanine aminotransferase and aspartate aminotransferase.
Very rare: hepatitis (including cholestatic, hepatocellular and mixed liver lesions).
Disorders of the skin and subcutaneous tissues:
Common: rash.
Uncommon: tendency to bruises, urticaria, itching.
Rarely: angioedema.
Very rare: erythema nodosum, erythema multiforme.
Musculoskeletal and connective tissue disorders:
Uncommon: arthralgia, myalgia, including muscle cramps.
Renal and urinary tract disorders:
Uncommon: enuresis in children.
General disorders and disorders at the injection site:
Common: pyrexia.
Uncommon: asthenia/fatigue, edema.
Interaction
Interaction
Montelukast can be prescribed together with other medicines that are usually used for the prevention and long-term treatment of bronchial asthma and/or the treatment of allergic rhinitis. The recommended therapeutic dose of montelukast did not have a clinically significant effect on the pharmacokinetics of the following drugs: theophylline, prednisone, prednisone, oral contraceptives (ethinyl estradiol/norethisterone 35/1), terfenadine, digoxin and warfarin.
The AUC value of montelukast is reduced by approximately 40% while taking phenobarbital, but this does not require changes in the dosage regimen of Almont.
In vitro studies have shown that montelukast inhibits the CYP2C8 isoenzyme of the cytochrome P450 system, however, in an in vivo drug interaction study between montelukast and rosiglitazone (metabolized by the CYP2C8 isoenzyme of the cytochrome P450 system), it was shown that montelukast did not inhibit the CYP2C8 isoenzyme. Thus, montelukast is not expected to influence the CYP2C8 isoenzyme-mediated metabolism of drugs (for example, paclitaxel, rosiglitazone, repaglinide).
In vitro studies have shown that montelukast is a substrate of the CYP2C8, 2C9 and 3A4 isoenzymes. Data from a clinical drug interaction study of montelukast and gemfibrozil (an inhibitor of both CYP2C8 and 2C9 isoenzymes) demonstrate that gemfibrozil increases the effect of systemic exposure to montelukast by 4.4 times. Co-administration of itraconazole, a potent inhibitor of the CYP3A4 isoenzyme, with gemfibrozil and montelukast did not lead to an additional increase in the effect of systemic exposure to montelukast. The effect of gemfibrozil on systemic exposure to montelukast may not be considered clinically significant based on the safety data for montelukast at doses greater than the approved dose of 10 mg in adults (no clinically significant adverse effects were observed at doses of 200 mg/day in adults for 22 weeks and up to 900 mg/day for approximately one week). Therefore, no dosage adjustment of montelukast is required when coadministered with gemfibrozil. Based on the results of in vitro studies, clinically significant drug interactions with other known inhibitors of the CYP2C8 isoenzyme (for example, trimethoprim) are not expected. In addition, coadministration of montelukast with itraconazole alone did not significantly increase the effect of systemic exposure to montelukast.
Combination treatment with bronchodilators
Almont is a reasonable addition to bronchodilator monotherapy if bronchodilators do not provide adequate control of bronchial asthma. Once the therapeutic effect of treatment with montelukast is achieved, a gradual reduction in the dose of bronchodilators can begin.
Combined treatment with inhaled glucocorticosteroids
Treatment with Almont provides an additional therapeutic effect for patients using inhaled glucocorticosteroids. Once the condition has stabilized, you can begin a gradual reduction in the dose of glucocorticosteroid under the supervision of a physician. In some cases, complete withdrawal of inhaled glucocorticosteroids is acceptable, but abrupt replacement of inhaled glucocorticosteroids with montelukast is not recommended.
Overdose
Overdose
Symptoms of drug overdose in patients with chronic bronchial asthma when used at a dose exceeding 200 mg per day for 22 weeks and at a dose of 900 mg per day for 1 week have not been identified.
There are reports of acute overdose of montelukast (when taking at least 1 g per day) in the post-registration period and in clinical studies in adults and children. Clinical and laboratory data indicate that the safety profile of the drug is consistent in children, adults and elderly patients. The most common symptoms were thirst, drowsiness, vomiting, psychomotor agitation, headache and abdominal pain.
Treatment: symptomatic therapy.
There are no data on the possibility of removing montelukast by peritoneal dialysis or hemodialysis.
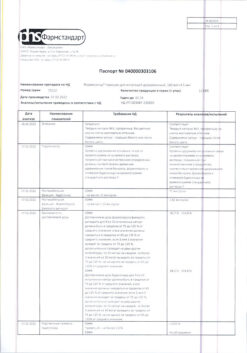
Storage conditions
Storage conditions
At a temperature not exceeding 25 C, in the original packaging. Keep out of the reach of children!
Shelf life
Shelf life
3 years.
Manufacturer
Manufacturer
Iceland
Additional information
| Shelf life | 3 years. |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 C, in the original package. Keep out of reach of children! |
| Manufacturer | Iceland |
| Medication form | pills |
Other forms…
Related products
Buy Almont, 10 mg 28 pcs. with delivery to USA, UK, Europe and over 120 other countries.