No products in the cart.
Advagraf, 1 mg 50 pcs
€1.00
Out of stock
(E-mail when Stock is available)
Description
The pharmacological action is immunosuppressive.
Pharmacodynamics
At the molecular level, the effects and intracellular cumulation of tacrolimus are due to binding to the cytosolic protein (FKBP 12). The FKBP 12-tacrolimus complex specifically and competitively inhibits calcineurin, providing calcium-dependent blocking of T-cell signaling pathways and preventing transcription of a discrete series of lymphokine genes.
Tacrolimus is a highly active immunosuppressant. In in vitro and in vivo experiments tacrolimus clearly reduced the formation of cytotoxic lymphocytes, which play a key role in the transplant rejection reaction. Tacrolimus suppresses the formation of lymphokines (IL-2, IL-3, γ-interferon), T-cell activation, IL-2 receptor expression, and T-helper-dependent B-cell proliferation.
Pharmacokinetics
Absorption
In humans, tacrolimus has been found to be rapidly absorbed in the GI tract. Advagraf®, sustained release capsules is a dosage form that provides prolonged absorption of tacrolimus in the GI tract. Average time to reach Cmax is about 2 hours. Absorption of tacrolimus is variable (absorption variability in adult patients is 6-43%). Bioavailability of tacrolimus when taken orally as capsules is on average 20-25%. Bioavailability, as well as the rate and degree of absorption of tacrolimus when concomitantly taken with food is reduced. The nature of biliary excretion does not affect absorption of the drug. Once the equilibrium concentration of tacrolimus is reached while taking Advagraf, there is a high correlation between AUC and minimum (C0) tacrolimus concentrations in blood. Therefore, monitoring of minimum (C0) tacrolimus concentrations in the blood provides an indication of systemic exposure to the drug.
Distribution and elimination
The distribution of tacrolimus in humans after IV administration is biphasic. In the systemic bloodstream, tacrolimus binds well to erythrocytes.
The ratio of tacrolimus concentrations in whole blood to plasma is approximately 20:1. A significant proportion of tacrolimus in plasma (>98.8%) is bound to plasma proteins (serum albumin, α1-acid glycoprotein).
Tacrolimus is widely distributed in the body. The steady-state volume of distribution taking into account plasma concentrations is about 1300 l (in healthy people). The same figure, calculated from whole blood, is on average 47.6 liters.
Tacrolimus is a substance with low clearance. In healthy people, the average total clearance calculated from whole blood concentrations is 2.25 L/h. In adult patients after liver, kidney, and heart transplantation, Cl values were 4.1; 6.7, and 3.9 L/h, respectively. Low hematocrit and hypoproteinemia contribute to an increase in the unbound fraction of tacrolimus, accelerating its clearance. Corticosteroids used in transplantation can also increase metabolic rate and accelerate tacrolimus clearance.
The half-life of tacrolimus is long and variable. In healthy subjects, the average T1/2 in whole blood is approximately 43 h.
Metabolism and biotransformation
Tacrolimus is actively metabolized in the liver, mainly by cytochrome P450 CYP3A4. Tacrolimus is metabolized intensively in the intestinal wall. Several metabolites of tacrolimus have been identified. In in vitro experiments it was shown that only one of the metabolites has immunosuppressive activity close to that of tacrolimus. Other metabolites were characterized by weak immunosuppressive activity or its absence. Only one of the tacrolimus metabolites was detected in the systemic bloodstream in low concentrations. Thus, the pharmacological activity of the drug is almost independent of the metabolites.
Excretion
After intravenous and oral administration of 14C-labeled tacrolimus, most of the radioactivity was detected in the feces. Approximately 2% of the radioactivity was detected in the urine. In the urine and feces, about 1% of tacrolimus was detected unchanged. Consequently, tacrolimus was almost completely metabolized before elimination: the main route of elimination was the biliary tract.
Indications
Indications
– prevention and treatment of hepatic, renal allograft rejection in adult patients;
– treatment of allograft rejection resistant to standard immunosuppressive therapy regimens in adult patients.
Active ingredient
Active ingredient
Composition
Composition
Active ingredient:
Tacrolimus (as tacrolimus monohydrate) 1 mg.
Auxiliary substances:
Hypromellose;
Ethylcellulose;
Lactose monohydrate;
Magnesium stearate.
Capsule shell:
titanium dioxide (E171);
iron oxide yellow dye (E172);
iron oxide red dye (E172);
gelatin;
sodium lauryl sulfate.
The inscription on the capsule (Opacode S-1-15083): pharmaceutical glaze 45% (shellac solution in ethanol); lecithin (soybean); simethicone; iron oxide red dye (E172); hyprolose
How to take, the dosage
How to take, the dosage
Ingestion. Advagraf® is an oral form of tacrolimus to be taken once daily. Advagraf therapy requires close monitoring by appropriately qualified and equipped personnel. Only physicians experienced in immunosuppressive therapy in transplant patients should prescribe this medication.
The uncontrolled transfer of patients from one tacrolimus medication to another (including switching from conventional capsules to prolonged capsules) is unsafe. This can lead to graft rejection or an increased incidence of side effects, including hypo- or hyperimmunosuppression, due to clinically significant differences in tacrolimus exposure. The patient should take one of the dosage forms of tacrolimus according to the recommended dosing regimen. A change in the dosage form or dosing regimen should only be made under the supervision of a transplant specialist. After transfer, tacrolimus blood concentrations should be monitored closely and the dose of the drug adjusted to maintain systemic tacrolimus exposure at an adequate level.
The initial doses presented below should be considered recommendations only. In the initial postoperative period, Advagraf® is usually used in combination with other immunosuppressants. The dose may vary depending on the immunosuppressive therapy regimen. The choice of a dose of Advagraf® should be based primarily on a clinical evaluation of the risk of rejection and individual tolerance of the drug, as well as on data of tacrolimus blood level monitoring (see section “Recommendations for monitoring therapeutic tacrolimus blood concentrations” below).
If clinical signs of rejection occur, consideration should be given to the need to adjust the immunosuppressive therapy regimen. In stable patients switched from Prograf (twice daily administration) to Advagraf® (once daily administration), with a total daily dose of 1:1 (mg:mg), systemic tacrolimus exposure (AUC0-24) was approximately 10% lower with Advagraf compared to Prograf. The relationship between minimum tacrolimus levels (C24) and systemic exposure to Advagraf was the same as with Prograf. When converting from Prograf to Advagraf®, minimum tacrolimus levels should be measured both before conversion from one drug to another and over the next 2 weeks. At the same time, Advagraf doses should be adjusted to achieve systemic tacrolimus exposure similar to Prograf.
In patients after de novo kidney and liver transplantation, the AUC0-24 of tacrolimus on the first day of use of Advagraf was 30 and 50% lower, respectively, compared with equivalent doses of Prograf.
By day 4, systemic tacrolimus exposure, as assessed by C0, was similar with Prograf and Advagraf in patients after liver and kidney transplantation. In order to ensure adequate tacrolimus exposure during Advagraf treatment during the first 2 weeks after transplantation, regular and careful monitoring of the minimum (C0) tacrolimus blood concentration is recommended. Since tacrolimus is a low clearance substance, it may take several days to reach equilibrium concentrations after Advagraf dose adjustment.
For patients who are unable to take the drug orally immediately after transplantation, tacrolimus may be administered by IV (Prograf 5 mg/ml, concentrate for infusion) at a dose that is approximately one-fifth of the recommended oral dose for the indication.
The oral daily dose of Advagraf is recommended to be taken in the morning once daily. Long-acting Advagraf capsules should be taken as soon as they are removed from the blister. Patients should be warned about the presence of a desiccant (sachet with silica gel) in the package, which is not intended to be taken. It is recommended to wash the capsules with liquid (preferably water). To achieve maximum absorption, it is recommended to take Advagraf® on an empty stomach: 1 hour or 2-3 hours after a meal. A missed dose should be taken as soon as possible, preferably the same day; do not take a double dose the next morning.
In order to prevent transplant rejection, immunosuppression must be maintained at all times; therefore, there is no limit to the duration of therapy.
Kidney transplantation
Prevention of transplant rejection
Advagraf oral therapy should be started with a daily dose of 0.2-0.3 mg/kg once daily in the morning. The drug should be started within 24 hours after transplantation.
Liver transplantation
Prevention of transplant rejection
Advagraf oral therapy should be started with a daily dose of 0.1-0.2 mg/kg once daily in the morning. The drug should be started 12-18 hours after transplantation.
Dose adjustments in the post-transplant period
Advagraf doses are usually reduced over time after kidney or liver transplantation. In some cases, withdrawal of concomitant immunosuppressants is possible, i.e. switching to Advagraf monotherapy. An improvement in the patient’s condition may alter the pharmacokinetics of tacrolimus and require additional adjustments to the doses of Advagraf.
Treatment of graft rejection
The following approaches are recommended to control graft rejection: increasing the dose of tacrolimus, increasing corticosteroid therapy, short courses of mono/polyclonal antibody therapy. If signs of tacrolimus toxicity occur (e.g., marked adverse reactions), doses of Advagraf may need to be reduced. For information on switching from cyclosporine to Advagraf® see “Conversion (transition) from cyclosporine to Advagraf®”.
Kidney and liver transplantation
When switching from other immunosuppressants to Advagraf®, treatment should begin with the initial oral doses described above in the sections “Prevention of Transplant Rejection” for kidney and liver transplantation.
Heart transplantation
When switching to therapy with Advagraf in adult patients, the initial oral daily dose of the drug is 0.15 mg/kg once daily in the morning.
Transplantation of other organs
There is no clinical experience with the use of Advagraf for treatment of patients after lung, pancreatic, or intestinal transplantation. However, tacrolimus (Prograf) is used in patients with lung transplants at an initial oral dose of 0.1-0.15 mg/kg/day, after pancreas transplantation at an initial oral dose of 0.2 mg/kg/day, after intestinal transplantation at an initial oral dose of 0.3 mg/kg/day.
Conversion (conversion) from cyclosporine to Advagraf®
Care should be taken when switching from cyclosporine to Advagraf®. Treatment with Advagraf is recommended to be initiated after determining the cyclosporine blood concentrations and evaluating the patient’s clinical condition. Conversion should be delayed in the presence of elevated blood levels of cyclosporine. In practice, tacrolimus therapy is initiated 12-24 h after discontinuation of cyclosporine. After conversion, it is recommended to monitor cyclosporine blood levels, since cyclosporine clearance may be delayed.
The conversion from Prograf to Advagraf®
If patients after allotransplantation who are taking Prograf twice daily are to be switched to taking Advagraf once daily, the daily dose ratio during conversion should be 1:1 (mg:mg). It is recommended to take Advagraf® in the morning. After switching to Advagraf® it is necessary to monitor minimum (C0) tacrolimus blood concentrations and make dose adjustments to maintain the systemic tacrolimus exposure at the same level.
Dose adjustments in selected patient categories
Patients with hepatic dysfunction. In patients with severe hepatic dysfunction, Advagraf dose reduction may be required to maintain minimum (C0) tacrolimus blood concentrations within the recommended therapeutic range.
Patients with renal dysfunction. Since renal function does not affect the pharmacokinetics of tacrolimus, there is no need to adjust doses. However, due to the nephrotoxic potential of tacrolimus, close monitoring of renal function (including determination of serum creatinine concentration, calculation of creatinine clearance and monitoring of urine output) is recommended.
Race. Black patients may require higher doses of tacrolimus than white patients to achieve similar minimum (C0) blood concentrations.
Gender. There is no evidence that males and females require different doses of the drug to achieve equal minimum (C0) tacrolimus blood concentrations.
Elderly patients. There is no evidence that elderly patients require specific doses of Advagraf.
Recommendations for Monitoring Therapeutic Blood Tacrolimus Concentrations
The choice of doses should be based on clinical assessment of individual risk of rejection and tolerability of the drug, as well as data on monitoring therapeutic tacrolimus blood levels.
To select the optimal dose, several methods are used to determine tacrolimus concentrations in whole blood. Comparisons between monitoring results published in the literature and monitoring results in an individual clinic should be made taking into account the method used to determine tacrolimus blood concentrations. In current clinical practice, tacrolimus blood levels are monitored primarily by immunoassay methods.
The correlation between minimum (C0, C24) concentrations and systemic exposure (AUC0-24) of tacrolimus in blood is the same with both drugs, Advagraf® and Prograf.
In the post-transplant period, close monitoring of minimum (C0, C24) tacrolimus concentrations in the blood is necessary. Minimum blood concentrations of Advagraf should be determined approximately 24 hours after administration of the drug, before the next dose. More frequent monitoring of minimum concentrations is recommended in the first 2 weeks after transplantation, followed by periodic monitoring during maintenance therapy. The therapeutic tacrolimus blood levels should be monitored carefully after conversion from Prograf to Advagraf®, when adjusting doses of drugs, when making changes in immunosuppressive therapy, or when concomitant use of drugs that may cause changes in tacrolimus blood concentrations (see sections “Conversion (transition) from cyclosporine to Advagraf®”, “Conversion (transition) from Prograf to Advagraf®” and “Interaction”). The frequency of monitoring blood drug levels is determined by clinical necessity. Because Advagraf® is a low clearance drug, it may take several days for tacrolimus blood concentrations to reach equilibrium levels after adjusting the Advagraf dose.
According to data from clinical studies, treatment is successful in most cases with therapeutic tacrolimus blood levels of 20 ng/mL or less. When interpreting data on therapeutic tacrolimus blood concentrations, the patient’s clinical condition must be taken into account.
It has been reported that in the initial post-transplant period in patients after liver transplantation the therapeutic blood levels of the drug are in the range of 5-20 ng/ml and after kidney or heart transplantation 10-20 ng/ml. During maintenance immunosuppressive therapy in patients after liver, kidney or heart transplantation, blood drug concentrations are usually in the range of 5-15 ng/ml.
Interaction
Interaction
Metabolic interactions
After oral administration, tacrolimus is metabolized in the intestinal cytochrome CYP3A4 system. Concomitant administration of drugs or herbs with an established inhibitory or inducing effect on CYP3A4 may respectively increase or decrease the blood concentration of tacrolimus. Therefore, to maintain adequate and consistent tacrolimus exposure, it is recommended that tacrolimus blood concentrations be monitored and the dose of Advagraf be adjusted as necessary.
Metabolic inhibitors. Based on clinical experience it was found that the following drugs can significantly increase tacrolimus blood concentrations: antifungal agents (ketoconazole, fluconazole, itraconazole, voriconazole), macrolide antibiotics (erythromycin), HIV protease inhibitors (ritonavir). When prescribing these drugs with tacrolimus, Advagraf doses may need to be reduced. Pharmacokinetic studies have shown that increased tacrolimus blood levels are primarily the result of increased oral bioavailability of the drug caused by inhibition of the intestinal metabolism of tacrolimus. Suppression of hepatic metabolism of tacrolimus plays a secondary role.
Less pronounced drug interactions were observed when tacrolimus was used simultaneously with clotrimazole, clarithromycin, josamycin, nifedipine, nicardipine, diltiazem, verapamil, danazol, ethinylestradiol, omeprazole and nefazodone.
The following substances have been shown in in vitro studies to be potential inhibitors of tacrolimus metabolism: bromocriptine, cortisone, dapsone, ergotamine, gestodine, lidocaine, mephenytoin, miconazole, midazolam, nilvadipine, noretinodron, quinidine, tamoxifen, (triacetyl) oleandomycin.
Grapefruit juice should also be avoided because of the possibility of elevated tacrolimus levels in the blood. Lansoprazole and cyclosporine may potentially inhibit CYP3A4-mediated metabolism of tacrolimus and increase its blood concentration.
Metabolism inducers. Based on clinical experience, it has been found that blood concentrations of tacrolimus can be significantly reduced by rifampicin, phenytoin and preparations of Hypericum perforatum. If these drugs are prescribed with tacrolimus, Advagraf doses may need to be increased.
Clinically significant interactions have been observed with phenobarbital.
Corticosteroids at maintenance doses usually decrease the blood concentration of tacrolimus. High doses of prednisolone or methylprednisolone used to treat acute rejection can increase or decrease tacrolimus blood levels.
Carbamazepine, methamizole and isoniazid can decrease tacrolimus blood concentrations.
The effect of tacrolimus on the metabolism of other drugs. Tacrolimus inhibits CYP3A4 and in concomitant administration may affect drugs metabolized in the CYP3A4 system. The elimination half-life of cyclosporine is prolonged when used concomitantly with tacrolimus. Synergistic/additive nephrotoxic effects may also be observed. For these reasons, concomitant administration of cyclosporine and tacrolimus is not recommended, and caution should be exercised when prescribing tacrolimus to patients who have previously taken cyclosporine.
Tacrolimus increases blood levels of phenytoin.
Because tacrolimus may decrease the clearance of hormonal contraceptives, it is important to use caution when choosing contraception.
The data on interactions of tacrolimus with statins are limited. Clinical observations suggest that the pharmacokinetics of statins are not altered by concomitant administration with tacrolimus.
Animal experimental studies have shown that tacrolimus has the potential to decrease clearance and increase the half-life of phenobarbital and antipyrine.
Other potential interactions that increase systemic exposure to tacrolimus include: prokinetics (metoclopramide, cisapride), cimetidine, magnesium and aluminum hydroxide.
Other potentially adverse drug interactions. Concomitant use of tacrolimus with drugs with nephro- or neurotoxicity (e.g., aminoglycosides, gyrase inhibitors, vancomycin, co-trimoxazole, NSAIDs, ganciclovir, acyclovir) may contribute to these effects.
Tacrolimus combined with amphotericin B and ibuprofen resulted in increased nephrotoxicity.
Because tacrolimus may contribute to or exacerbate hyperkalemia, high doses of potassium or potassium-saving diuretics (amiloride, triamterene, spironolactone) should be avoided.
The immunosuppressants may change the body’s response to vaccination: vaccination during treatment with tacrolimus may be less effective. Live, attenuated vaccines should be avoided.
Protein binding. Tacrolimus actively binds to plasma proteins. Possible competitive interaction of tacrolimus with drugs with high affinity for blood plasma proteins (NSAIDs, oral anticoagulants, oral antidiabetic agents) should be considered.
Incompatibilities. Tacrolimus is incompatible with polyvinyl chloride (PVC). Test tubes, syringes and other equipment used when preparing a suspension of Advagraf capsules must not contain PVC.
Special Instructions
Special Instructions
There is limited experience in the treatment of non-white race and high immunologic risk patients (i.e., repeat transplant, high panel reactive antibody titer – PRA). There are no clinical data on the use of Advagraf in acute rejection refractory to therapy with other immunosuppressants in adult patients.
There are currently no clinical data on the use of Advagraf for the prevention of transplant rejection in heart transplant and pediatric patients.
In the initial post-transplant period the following parameters should be monitored regularly: BP, ECG, neurological and visual status, fasting glycemia, electrolytes concentration (especially potassium), hepatic and renal function parameters, hematologic parameters, coagulogram, proteinemia level. In the presence of clinically significant changes correction of immunosuppressive therapy is necessary.
When using Advagraf, prescription of herbal preparations containing Hypericum perforatum and other herbal agents which may cause decrease (change) of tacrolimus concentration in blood and have adverse effect on the clinical effect of Advagraf should be avoided.
In diarrhea, tacrolimus blood levels may change significantly; close monitoring of tacrolimus blood concentrations is necessary if diarrhea occurs.
The concomitant use of cyclosporine and tacrolimus should be avoided, and care should be taken when treating patients who have previously received cyclosporine with tacrolimus (see “Conversion (transition) from cyclosporine to Advagraf®”).
Cases of ventricular or septal hypertrophy reported as cardiomyopathy are rare but have been observed in patients receiving Prograf and are therefore possible with Advagraf treatment. Myocardial hypertrophy was reversible in most cases and was observed at blood concentrations (C0) of tacrolimus higher than recommended. Other factors that increase the risk of this adverse event include: previous heart disease, corticosteroid use, arterial hypertension, renal and hepatic dysfunction, infections, hypervolemia, edema. High-risk patients receiving intensive immunosuppressive therapy should have echocardiographic and ECG monitoring before and after transplantation (at 3 and 9-12 months). If abnormalities are detected, consideration should be given to reducing the dose of Advagraf or replacing the drug with another immunosuppressant.
Tacrolimus may cause prolongation of the QT interval, and no pirouette-type heart rhythm disturbances (bidirectional spindle-shaped ventricular tachycardia) have been observed. Special caution should be exercised when treating patients with diagnosed or suspected congenital long QT interval syndrome.
Patients treated with tacrolimus may develop post-transplant lymphoproliferative diseases (PTLD) associated with Epstein-Barr virus. The concomitant use of the drug with anti-lymphocyte antibodies increases the risk of PTLD. There are also reports of an increased risk of PTLD in patients with detected Epstein-Barr virus capsid antigen. Therefore, serological testing for Epstein-Barr virus capsid antigen should be performed before prescribing Advagraf in this group of patients. Close monitoring for Epstein-Barr virus by polymerase chain reaction (PCR) is recommended during treatment. A positive PCR for Epstein-Barr virus may persist for months and is not in itself evidence of PTLD or lymphoma.
Patients receiving immunosuppressive therapy, including Advagraf®, are at increased risk of opportunistic infections (caused by bacteria, fungi, viruses, protozoa). Among these infections, VC-virus-associated nephropathy and JC-virus-associated progressive multifocal leukoencephalopathy (PML) are noted. These infections are often associated with profound immune system suppression and can lead to severe or fatal outcomes, which must be taken into account when making a differential diagnosis in patients who have signs of renal dysfunction or neurological symptoms on immunosuppressive therapy.
Immunosuppressive therapy increases the risk of malignancy. It is recommended to limit insolation and UV exposure, wear appropriate clothing, and use sunscreens with a high protection factor.
The risk of developing secondary cancer is unknown.
There have been reports of reversible posterior encephalopathy syndrome on tacrolimus therapy. If a patient taking tacrolimus develops symptoms characteristic of reversible posterior encephalopathy syndrome – headache, mental disturbances, seizures and visual disturbances – an MRI should be performed. If the diagnosis is confirmed, BP and seizures should be adequately controlled, and systemic tacrolimus administration should be stopped immediately. If these measures are taken, the condition is completely reversible in most patients.
Because Advagraf sustained release capsules contain lactose, special caution should be exercised when prescribing the drug in patients with rare hereditary conditions associated with galactose intolerance, Lapp lactase deficiency or glucose-galactose malabsorption.
Impact on the ability to drive and operate machinery
Tacrolimus may cause visual and neurological impairment, especially when Advagraf is combined with alcohol.
Contraindications
Contraindications
Side effects
Side effects
Because of the nature of the underlying disease and the large number of medications used simultaneously after transplantation, the profile of immunosuppressant adverse events is difficult to establish accurately.
Many of the adverse events presented below are reversible and/or decrease with dose reduction. Within each frequency group, adverse events are presented in descending order of severity. The adverse events, classified by organs and systems, are listed below in descending order of frequency of occurrence: very common – >1/10), common – â¥1/100 to <1/10; infrequent – â¥1/1000 to <1/100; rare – â¥1/10000 to <1/1 000; very rare – <1/10000); unknown (for which there are not enough data to establish frequency).
Heart: frequent – coronary coronary disorders, tachycardia; infrequent – ventricular arrhythmias and cardiac arrest, heart failure, cardiomyopathy, ventricular hypertrophy, supraventricular arrhythmias, palpitations, abnormal ECG values, heart rhythm, HR and pulse disorders; rare – pericardial effusion; very rare – abnormal echocardiogram values.
Blood and lymphatic system: frequently – anemia, leukopenia, thrombocytopenia, leukocytosis; infrequently – coagulopathy, abnormal coagulogram, pancytopenia, neutropenia; rarely – thrombotic thrombocytopenic purpura, hypoprothrombinemia.
Nervous system: very common – tremor, headache; common – epileptoid seizures, impaired consciousness, paresthesias and dysesthesias, peripheral neuropathies, dizziness, writing disorders, nervous system disorders; infrequent – coma, CNS hemorrhage and cerebral circulation disorders, paralysis and paresis, encephalopathy, speech and articulation disorders, amnesia; rare – increased muscle tone; very rare – myasthenia gravis.
VIight organs: often – blurred vision, photophobia, eye disease; infrequently – cataracts; rarely – blindness.
Hearing and balance organs: often – tinnitus (ringing) in the ears; infrequent – decreased hearing; rare – neurosensory deafness; very rare – hearing disorders.
Respiratory system and mediastinum: often – shortness of breath, pulmonary parenchymal disorders, pleural effusion, pharyngitis, cough, nasal congestion, rhinitis; infrequent – respiratory failure, airway disorders, asthma; rarely – acute respiratory distress syndrome.
Gastrointestinal disorders: very often – diarrhea, nausea; common – inflammatory gastrointestinal disorders, gastrointestinal ulcers and perforations, gastrointestinal bleeding, stomatitis and oral mucosal ulceration, ascites, vomiting, gastrointestinal and abdominal pain, dyspepsia, constipation, flatulence, feeling of bloating and distention in the stomach, liquid stool, infrequently – paralytic ileus, peritonitis, acute and chronic pancreatitis, increased blood amylase levels, gastroesophageal reflux disease, disorders of gastric evacuation function, rarely – subileus, pancreatic pseudocysts.
Kidney and urinary tract: very common – renal dysfunction; common – renal failure, including acute, oliguria, acute tubular necrosis, toxic nephropathy, urinary syndrome; infrequent – anuria, hemolytic uremic syndrome; very rare – nephropathy, hemorrhagic cystitis.
The skin and subcutaneous tissue: frequently – itching, rash, alopecia, acne, hyperhidrosis, infrequently – dermatitis, photosensitization, rarely – toxic epidermal necrolysis (Lyell’s syndrome), very rarely – Stevens-Johnson syndrome.
Muscular system and connective tissue: often – arthralgia, muscle cramps, pain in the extremities, back pain; infrequent – joint disorders.
Endocrine system: rarely – hirsutism.
Metabolism and nutrition: very common – hyperglycemia, diabetes mellitus, hyperkalemia; common – hypomagnesemia, hypophosphatemia, hypokalemia, hypocalcemia, hyponatremia, hypervolemia, hyperuricemia, decreased appetite, anorexia, metabolic acidosis, hyperlipidemia, hypercholesterolemia, hypertriglyceridemia, electrolyte disorders; infrequently – dehydration, hypoproteinemia, hyperphosphatemia, hypoglycemia.
Immune system: during therapy with tacrolimus, as well as other immunosuppressants, the risk of local and generalized infectious diseases (viral, bacterial, fungal, protozoal) increases. The course of previously diagnosed infectious diseases may worsen. Cases of BC-virus-associated nephropathy and progressive multifocal leukoencephalopathy (PML) associated with JC-virus have been observed on immunosuppressive therapy, including Advagraf therapy.
Injuries, poisonings, complications of procedures: often primary graft dysfunction.
Benign, malignant and unidentified neoplasms. Patients receiving immunosuppressive therapy have a higher risk of malignancy. Both benign and malignant neoplasms, including Epstein-Barr virus (EBV)-associated lymphoproliferative disease and skin cancer, have been reported with tacrolimus.
Vascular system: very common – arterial hypertension; common – bleeding, thromboembolic and ischemic complications, peripheral circulatory disorders, arterial hypotension; infrequent – infarction, deep vein thrombosis of extremities, shock.
General disorders and complications: frequent – asthenia, febrile states, edema, pain and discomfort, increased levels of alkaline phosphate in the blood, weight gain, disorders of body temperature perception; infrequent – multiple organ failure, flu-like syndrome, abnormal perception of ambient temperature, feeling of tightness in the chest, anxiety, worsening of well-being, increased blood lactate dehydrogenase level, weight loss; rare – thirst, loss of balance (falling), feeling of stiffness in the chest, difficulty in movement; very rare – increase in adipose tissue mass.
The immune system (allergic reactions). Allergic and anaphylactic reactions have been observed in patients taking tacrolimus.
The liver and biliary tract: often – increased liver enzymes, liver dysfunction, cholestasis and jaundice, liver cell damage and hepatitis, cholangitis; rarely – hepatic artery thrombosis, obliterating endophlebitis of liver veins; very rarely – liver failure, bile duct stenosis.
Reproductive system and the mammary glands: infrequent – dysmenorrhea and uterine bleeding.
Fertility. Negative effects of tacrolimus on male fertility, expressed in decreased sperm count and motility, have been found in rats.
Mental sphere: very common – insomnia; common – anxiety, confusion and disorientation, depression, depressed mood, emotional disturbances, nightmares, hallucinations, psychotic disorders; infrequent – psychotic disorders.
Overdose
Overdose
The information on overdose is limited. Several episodes of accidental overdose have been reported in patients taking tacrolimus. Symptoms have included tremors, headache, nausea, vomiting, infections, urticaria, lethargy, elevated blood urea nitrogen, serum creatinine and alanine aminotransferase.
There are currently no antidotes to tacrolimus. In case of overdose, standard measures should be taken and symptomatic treatment should be administered.
With regard to the high molecular weight of tacrolimus, poor water solubility and marked binding to erythrocytes and plasma proteins, dialysis is ineffective. Hemofiltration or diafiltration were effective in individual patients with very high concentrations of tacrolimus in the blood. In cases of oral overdose, gastric lavage and/or the use of adsorbents (e.g. activated charcoal) may be effective if these measures are taken soon after taking the drug.
Pregnancy use
Pregnancy use
Pregnancy
The results of preclinical and clinical studies indicate that the drug may penetrate the placenta. There have been reports of preterm delivery (< 37 weeks), as well as cases of spontaneously resolved hyperkalemia in neonates (8 of 111 (7.2%) neonates). Since the safety of tacrolimus in pregnant women has not been sufficiently established, the drug is taken during pregnancy only when there is no safer alternative and when the benefit of treatment justifies the potential risk to the fetus. In order to detect potential adverse reactions of tacrolimus, it is recommended to monitor neonates whose mothers have taken tacrolimus during pregnancy (in particular, to pay attention to renal function).
Lactation period
According to clinical experience, tacrolimus penetrates into breast milk. Since it is not possible to rule out adverse effects of tacrolimus on the newborn, women taking Advagraf® should refrain from breastfeeding.
Similarities
Similarities
Additional information
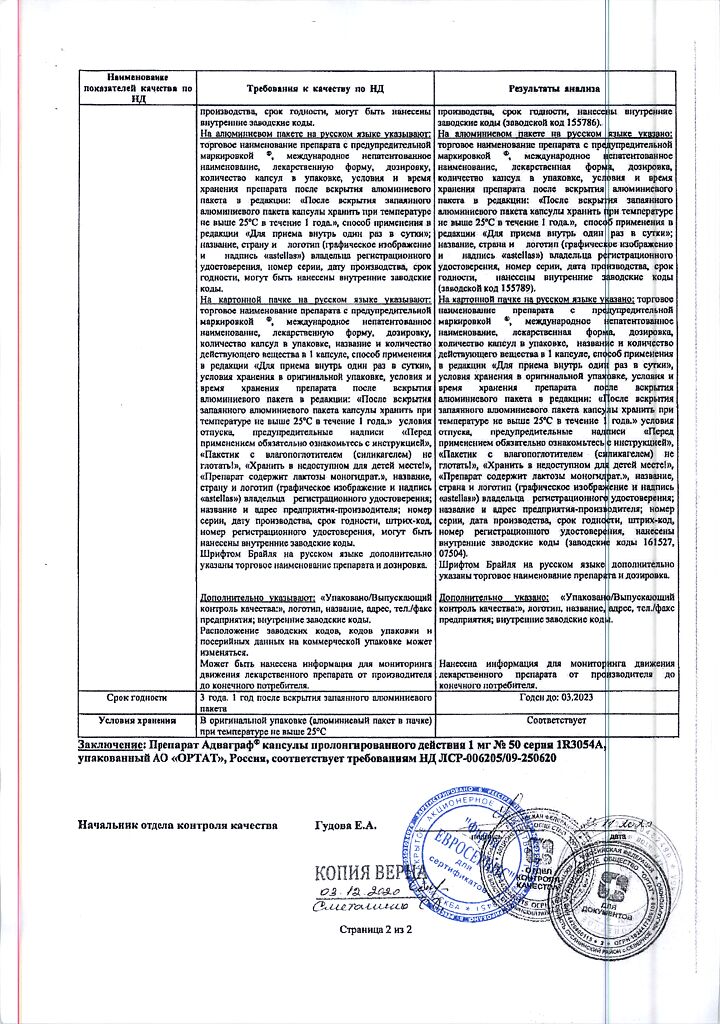
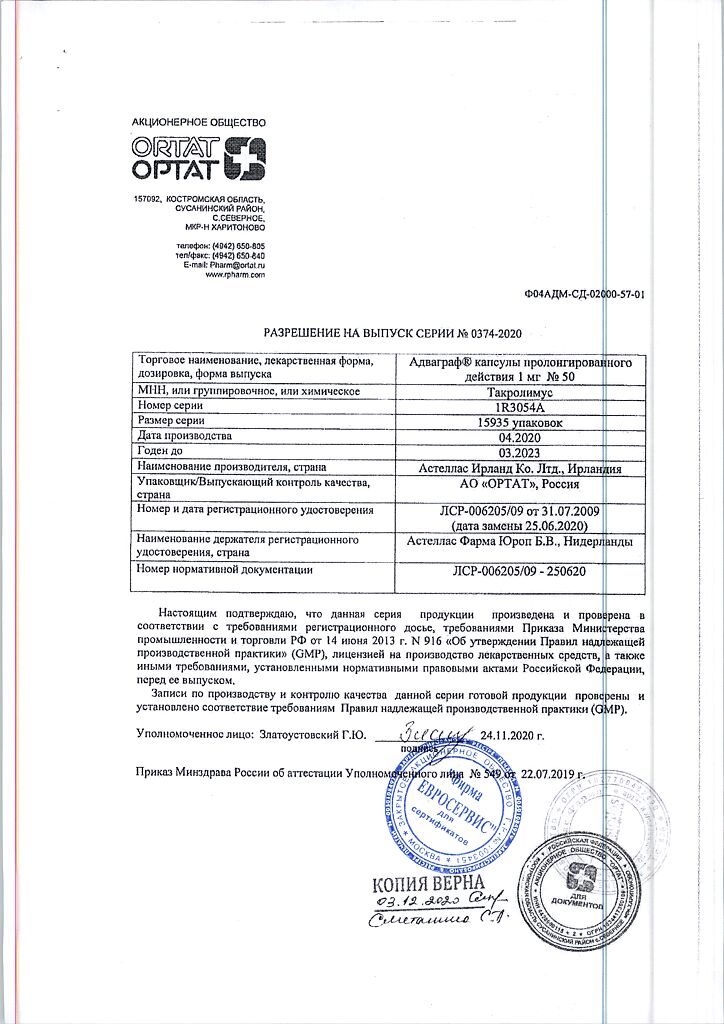
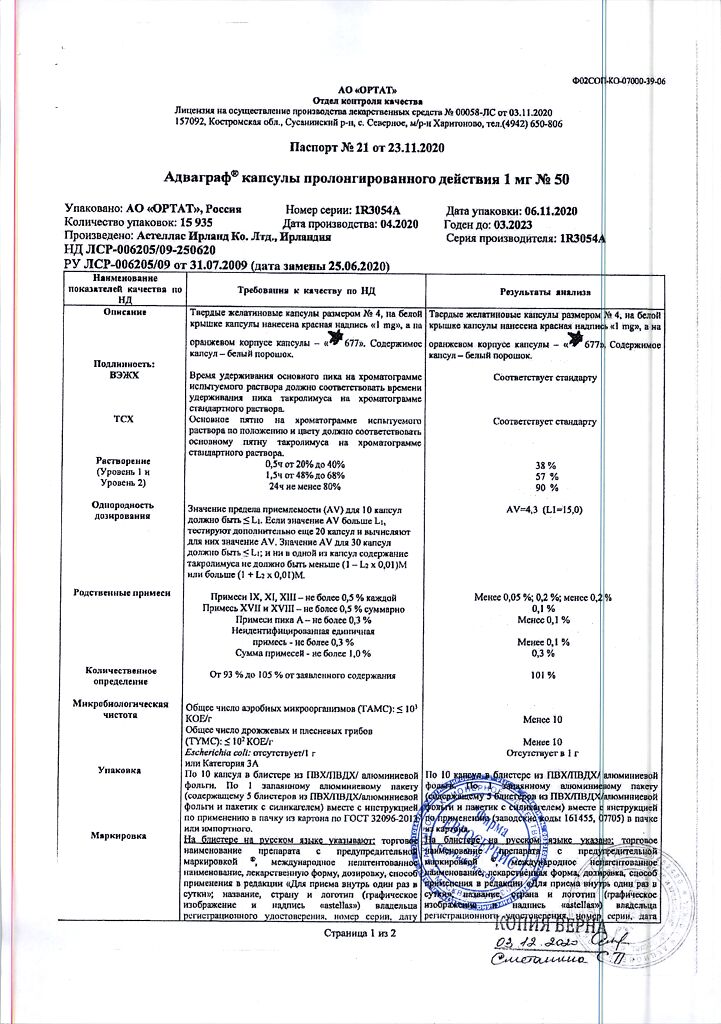
| Shelf life | 3 years |
|---|---|
| Conditions of storage | At a temperature not exceeding 25 °C, in the original package |
| Manufacturer | Astellas Ireland Co. |
| Medication form | slow-release capsules |
| Brand | #Н/Д |
Related products
Buy Advagraf, 1 mg 50 pcs with delivery to USA, UK, Europe and over 120 other countries.