No products in the cart.
Description
Pharmacotherapeutic group:
Antitumor agent – alkaloid
ATC:
L.01.C.D Taxoids
L.01.C.D.01 Paclitaxel
Pharmacodynamics:
The mechanism of action of paclitaxel is based on its ability to stimulate mitotic spindle microtubule assembly from dimeric tubulin molecules and stabilize microtubules by inhibiting their depolymerization. This leads to suppression of the normal dynamic reorganization of the microtubule network in the interphase of mitosis and causes formation of abnormal clusters of microtubules throughout the cell cycle and the appearance of multiple star-shaped clusters (asters) in the mitosis phase.
Abraxane contains nanodispersed paclitaxel stabilized by albumin with nanoparticle size of approximately 130 nm with paclitaxel in non-crystalline (amorphous) state.
After intravenous injection the nanoparticles rapidly dissociate to form soluble paclitaxel complexes bound to albumin with the approximate size of 10 nm.
Albumin is known to regulate the transendothelial transport of plasma components and in in vitro studies it was demonstrated that the presence of albumin in Abraxane stimulates the transport of paclitaxel through the endothelial cell layer.
It has been hypothesized that transendogelial transport is mediated by the albumin transporter gp-60, and there is increased cumulation of paclitaxel in the tumor due to the albumin-binding protein, an acidic secreted protein rich in cysteine (SPARC).
Pharmacokinetics:
The pharmacokinetics (PK) of paclitaxel have been studied in clinical studies at 30-minute and 180-minute infusions of Abraxane at doses ranging from 80 to 375 mg/m2. The area under the concentration-time curve (AUC) values for paclitaxel increased linearly, from 2653 ng*h/mL to 16736 ng*h/mL, over a dose range of 80 to 300 mg/m2.
In a study involving patients with advanced solid tumors, paclitaxel FC parameters after an IV infusion of Abraxane at a dose of 260 mg/m2 for 30 minutes were compared with FC parameters after a solvent-based paclitaxel infusion at a dose of 175 mg/m2 for 3 hours.
Based on the uncompartmentalized analysis, paclitaxel clearance (43%) and volume of distribution (53%) were higher with administration of Abraxane than with solvent-based paclitaxel. No differences in terminal elimination half-life were reported.
In a study of multiple IV administration of Abraxane at a dose of 260 mg/m2 to 12 patients, intraindividual variability in paclitaxel systemic exposure (AUC) values was 19% (range of values = 3.21%-27.70%). No signs of paclitaxel cumulation were registered during several courses of therapy.
Distribution
After administration of Abraxane to patients with solid tumors paclitaxel was evenly distributed in blood cells and plasma and was 94% bound to plasma proteins.
The binding of paclitaxel to proteins was assessed by ultrafiltration in a comparison study in the same patient. The fraction of free paclitaxel was significantly higher with Abraxane (6.2%) than with solvent-based paclitaxel (2.3%).
This provided significantly higher exposure values of the unbound fraction of paclitaxel when administered with Abraxane than with solvent-based paclitaxel, even with comparable values of total exposure.
This phenomenon is probably due to the lack of paclitaxel binding to Cremophor EL micelles that is observed with solvent-based paclitaxel.
According to published studies that evaluated in vitro binding of paclitaxel (at concentrations from 0.1 to 50 µg/ml) to human plasma proteins, the presence of cimetidine, ranitidine, dexamethasone or diphenhydramine had no effect on paclitaxel binding to plasma proteins.
Given the results of a population-based analysis of FC data, the total volume of distribution is approximately 1,741 L; the high volume of distribution indicates intensive extravascular distribution and/or binding of paclitaxel to tissue proteins.
Metabolism and excretion
In in vitro studies using liver microsomes and human tissue slices have shown that paclitaxel is metabolized predominantly to form 6α-hydroxypaclitaxel and two additional metabolites present in smaller amounts (3′-n-hydroxypaclitaxel and 6α-3′-n-dihydroxypaclitaxel).
The formation of these hydroxylated metabolites is catalyzed by cytochrome P450 system isoenzymes CYP2C8, CYP3A4, and both CYP2C8 and CYP3A4, respectively.
In patients with metastatic breast cancer, after IV drip administration of Abraxane for 30 minutes at a dose of 260 mg/m2, the mean cumulative urinary excretion of unchanged active ingredient corresponded to 4% of the total drug dose administered; less than 1% of the administered dose accounted for the urinary excreted metabolites 6α-hydroxypaclitaxel and 3′-n-hydroxyaclntaxel, indicating significant extrarenal clearance of the drug.
Paclitaxel is predominantly eliminated by hepatic metabolism and excretion with bile.
When administered at a therapeutic dose of 80 to 300 mg/m2, mean plasma clearance of Paclitaxel ranges from 13 to 30 L/h/m2 and mean terminal elimination half-life ranges from 13 to 27 hours.
Hepatic dysfunction
The results of clinical studies have demonstrated that mild hepatic impairment (total bilirubin >1 to ≤1.5 x upper limit of normal, VGN) had no clinically significant effect on paclitaxel FC parameters.
In patients with moderate hepatic impairment (total bilirubin >1.5 to ≤3 x HGN) and severe impairment (total bilirubin >3 to ≤5 x HGN), there was a 22%-26% decrease in the maximum paclitaxel elimination rate and an approximately 20% increase in mean paclitaxel AUC.
Hepatic insufficiency had no effect on the mean Cmax value of paclitaxel. In addition, paclitaxel elimination was inversely correlated with the values of total bilirubin, and directly correlated with the values of plasma albumin concentration.
Pharmacokinetic/pharmacodynamic modeling showed no correlation between liver function (as measured by baseline albumin or total bilirubin concentration) and neutropenia with regard to Abraxane exposure.
FC analysis was not performed in patients with total bilirubin >5 x VGN or patients with metastatic pancreatic adenocarcinoma (see section “Dosage and administration”).
Renal dysfunction
Mild to moderate renal impairment (creatinine clearance ≥30 to <90 mL/min) had no clinically significant effect on the maximum elimination rate and systemic exposure (AUC and Cmax) of paclitaxel.
There are insufficient pharmacokinetic analysis data for patients with severe renal impairment and no data for patients with end-stage renal failure.
Elderly patients
A population-based analysis of the FC of Abraxane included data from patients aged 24 to 85 years. The results showed that age had no significant effect on the maximum elimination rate and systemic exposure (AUC and Cmax) of paclitaxel.
Pharmacokinetic/pharmacodynamic modeling using data from 125 patients with advanced solid tumors showed that patients aged ≥65 years may be more prone to develop neutropenia during the first cycle of therapy, although age had no effect on plasma paclitaxel exposure.
Other Intrinsic Factors
A population-based FC analysis of Abraxane demonstrated that gender, race (Mongoloid versus Caucasoid), and type of solid tumors had no clinically significant effect on systemic exposure (AUC and Cmax) to paclitaxel. The AUC of paclitaxel in patients with a body weight of 50 kg is approximately 25% lower than in patients with a body weight of 75 kg. The clinical significance of these data is unknown.
Indications
Indications
Active ingredient
Active ingredient
Composition
Composition
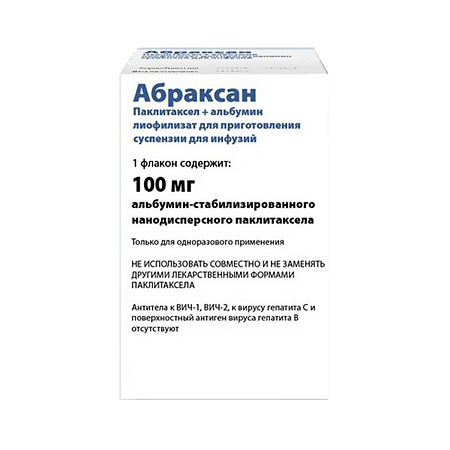
1 vial contains:
Paclitaxel 100 mg,
Human albumin 900 mg.
How to take, the dosage
How to take, the dosage
Abraxane should only be administered under the supervision of a qualified oncologist in departments designated for treatment with cytotoxic drugs. The drug should not be substituted for or used with other dosage forms of paclitaxel.
Breast cancer
Abraxan is administered by IV drip for 30 minutes at a dose of 260 mg/m2 once every 3 weeks.
Changing the dose of the drug in the treatment of breast cancer
If severe neutropenia (neutrophil count less than 500/μL for 1 week or more) or severe sensory neuropathy develops, the dose of Abraxane should be reduced to 220 mg/m2 for all subsequent courses of therapy.
If severe neutropenia or severe sensory neuropathy reoccur, the dose should be reduced to 180 mg/m2.
Abraxan should not be used until the neutrophil count has recovered to above 1,500/μL and the platelet count to above 100,000/mm3. In patients with grade 3 sensory neuropathy, treatment should be suspended until neuropathy is reduced to grade 1 or 2, with subsequent reduction in the dose of Abraxane for all subsequent courses of therapy.
Pancreatic adenocarcinoma
Abraxane in combination with gemcitabine is administered by IV. Abraxane at a dose of 125 mg/m2 is given for 30 minutes on days 1, 8, and 15 of each 28-day cycle. Gemcitabine at the recommended dose of 1000 mg/m2 is given for 30 minutes immediately after completion of Abraxane, on days 1, 8 and 15 of each 28-day cycle.
Particular patient groups
Patients with mild hepatic impairment (total bilirubin >1 to â¤1.5ÃVGN and AST â¤10ÃVGN) do not require dose changes, regardless of indication. The same doses of the drug should be used as in patients with normal liver function.
In patients with metastatic breast cancer with moderate to severe hepatic impairment (total bilirubin >1.5 to â¤5ÃVGN and AST â¤10ÃVGN), a 20% dose reduction is recommended. This reduced dose can be increased to the normal therapeutic dose (as in patients with normal liver function) if the patient has tolerated the first two cycles of therapy well.
For patients with metastatic pancreatic adenocarcinoma and moderate to severe hepatic dysfunction, there are insufficient data to make recommendations regarding dose changes for Abraxane.
For patients with a total bilirubin concentration of >5ÃVGN and AST activity of >10ÃVGN, regardless of indication, there is insufficient data to make dosing recommendations.
In patients with mild to moderate renal impairment (CK â¥30 to <90 ml/min), a change in the starting dose of Abraxane is not required. There are insufficient data to develop dosing recommendations for patients with severe and terminal (CK <30 ml/min) renal failure.
The safety and efficacy of Abraxane in children and adolescents under 18 years of age have not been studied. There are no data on the use of Abraxane in pediatric patients with breast cancer or pancreatic adenocarcinoma.
There is no additional dose reduction for patients 65 years of age or older beyond that recommended for all patients.
A patient with pancreatic adenocarcinoma aged 75 years and older should be carefully evaluated before therapy is prescribed.
An analysis of pharmacokinetic/pharmacodynamic modeling data for 125 patients with advanced solid tumors indicates that the risk of neutropenia during the first two cycles of therapy may be higher in patients 65 years and older.
Preparing the drug for administration
The reconstituted suspension of Abraxane is administered intravenously, using an infusion system with a built-in 15 µm pore diameter filter.
With respect to asepsis, prepare the suspension for infusion as follows:
1. Remove the protective cap from the bottle, wipe the stopper with an alcohol solution.
2. Using a sterile syringe, slowly (for at least 1 minute) inject 20 ml of 0.9% sodium chloride solution for injection into the vial. The needle of the syringe should be directed in such a way that the solution flows down the wall of the vial.
3 To prevent foaming, avoid applying the solution directly to the lyophilizate.
4 Once all of the saline solution has been infused into the vial, leave it for at least 5 minutes to allow the solution to be absorbed evenly by the lyophilizate.
5. Gently rotate and/or invert the vial for at least 2 minutes to ensure that the lyophilizate completely and evenly dissolves in the volume of sodium chloride solution injected to form a homogeneous suspension. Do not allow foaming.
6 If foam or agglomerates form, leave the vial for at least 15 minutes until the foam has completely settled. If necessary, repeat dissolving until agglomerates have disappeared.
7. The ready to use preparation is a homogenous translucent suspension of white or white with yellowish tinge without visible mechanical inclusions. Some sedimentation of the reconstituted suspension is allowed.
If there is sediment before the drug is administered, the homogeneity of the suspension should be achieved by gently turning the bottle again. Before administration, the suspension should be inspected to see if there are any visible mechanical particles in it. If such particles are found, the reconstituted suspension should not be injected.
8. Each mL of the reconstituted suspension contains 5 mg of albumin-stabilized nanodispersed paclitaxel (no further dilution is required prior to administration). The total volume of the suspension for infusion is calculated as follows: infusion volume (ml) = total dose (mg)/5 (mg/ml).
9. Transfer the prepared suspension in the required volume corresponding to the calculated drug dose to an empty standard PVC (or PVC-free) infusion bag.
The use of medical devices (in particular syringes and infusion bags) that use silicone oil as a lubricant for reconstitution and administration of Abraxane may result in the formation of protein “threads”.
In this regard, to eliminate the possibility of such protein “threads” entering the bloodstream, infusion of Abraxane should be carried out using a built-in filter with a pore size of 15 µm. Such a filter removes these particles without changing the physical and chemical characteristics of the reconstituted suspension of the drug.
The use of a smaller pore size than 15 µm can cause the filter to become clogged and blocked.
With the potential for vascular contamination, the administration of the product should be monitored closely to detect possible symptoms of infiltration at the site of the IV injection in a timely manner.
Limiting the time of administration of Abraxane to 30 minutes, as recommended, reduces the likelihood of adverse reactions at the site of infusion.
Interaction
Interaction
Special studies of interaction of Abraxane with other drugs have not been conducted.
. Due to the fact that metabolism of paclitaxel is partially mediated by CYP2C8 and CYP3A4 isoenzymes of cytochrome P450 system, the drug Abraxane should be used with caution in combination with inhibitors of these isoenzymes (including ketoconazole and other antifungal agents – imidazole derivatives, erythromycin, fluoxetine, gemfibrozil, cimetidine, ritonavir, saquinavir, indinavir and nelfinavir) or inducers of these isoenzymes (including rifampicin, carbamazepine, phenytoin, efavirenz, nevirapine).
Paclitaxel and gemcitabine have different metabolic pathways.
The clearance of paclitaxel is primarily due to metabolism catalyzed by CYP2C8 and CYP3A4 isoenzymes, with subsequent excretion in the bile; gemcitabine is inactivated by cytidine deaminase, with subsequent excretion in the urine.
There have been no studies of pharmacokinetic interaction of Abraxane and gemcitabine in humans.
The drug Abraxane is indicated as monotherapy of breast cancer, or in combination with gemcitabine for treatment of pancreatic adenocarcinoma. Abraxane should not be combined with other anticancer drugs.
Special Instructions
Special Instructions
Abraxane should only be administered under the supervision of a physician experienced in the use of antitumor drugs and under the conditions necessary to control possible complications.
Abraxan should not be mixed with any drugs other than those listed under “Preparation of the drug for intravenous administration”.
Hypersensitivity
In rare cases severe hypersensitivity reactions have been reported, including very rare anaphylactic reactions with fatal outcome. If the patient showed symptoms of hypersensitivity the drug should be immediately discontinued without further resumption. The patient should be prescribed symptomatic therapy.
Hematological toxicity
Suppression of bone marrow function (mainly neutropenia) during treatment with Abraxane is common. Neutropenia is dose-dependent and is the main factor limiting the dose of the drug.
Peripheral blood counts should be monitored regularly during treatment with Abraxane.
Retreatment with Abraxane should be repeated only when the neutrophil count is above 1500/mm3 and the platelet count is above 100,000/mm3.
Neuropathy
In treatment with Abraxane sensory neuropathy often develops and less often its severe forms.
In cases of sensory neuropathy of severity 1 or 2, it is usually not necessary to reduce the dose of the drug.
In case of development of severe sensory neuropathy (3rd degree of severity) during monotherapy with Abraxane, treatment should be suspended until relief of symptoms to degree 1-2 and the dose of Abraxane should be reduced in all subsequent courses.
If sensory neuropathy of grade â¥3 develops on combination therapy with Abraxane and gemcitabine, the administration of Abraxane should be delayed while continuing therapy with gemcitabine at the same dose.
Abraxane therapy at a reduced dose should be resumed when the severity of peripheral neuropathy has decreased to grade 0 or 1.
Sepsis
Sepsis has been reported in 5% of patients treated with Abraxane in combination with gemcitabine regardless of the presence of neutropenia.
Complications of pancreatic cancer, particularly biliary obstruction and the presence of a biliary stent, were major risk factors for sepsis.
If the patient has an elevated body temperature (regardless of the neutrophil count), therapy with broad-spectrum antibiotics should be initiated.
In case of febrile neutropenia the administration of Abraxane and gemcitabine should be delayed until the body temperature normalizes and the absolute neutrophil count is restored to â¥1500 cells/mm3, and then the treatment with both drugs should be resumed at reduced dose.
Pneumonitis
Pneumonitis has been reported in 4% of patients treated with Abraxane in combination with gemcitabine. Of the 17 cases of pneumonitis, 2 ended lethally.
Patients should be closely monitored for timely detection of signs and symptoms of pneumonitis.
Once infectious etiology of the disease has been ruled out and the diagnosis of pneumonitis has been confirmed, treatment with Abraxane and gemcitabine must be withdrawn (without possibility of relapse), and appropriate treatment and supportive measures must be initiated immediately.
Hepatotoxicity
Because patients with impaired liver function have an increased likelihood of paclitaxel toxicity, Abraxane should be used with caution in them.
Because of the higher risk of toxic reactions, especially myelosuppression, the blood count should be monitored in patients with impaired liver function.
The drug Abraxane should not be used in patients with bilirubin >5ÃVGN or AST >10ÃVGN concentrations. In addition, Abraxane is not recommended for use in patients with metastatic pancreatic adenocarcinoma with moderate to severe hepatic impairment (total bilirubin >1.5ÃVGN and AST â¤10ÃVGN).
Cardiotoxicity
In patients receiving Abraxane, single cases of congestive heart failure and left ventricular dysfunction have been reported. At the same time, most patients had a history of heart disease or use of cardiotoxic agents such as anthracyclines.
Patients receiving Abraxane should therefore be kept under constant medical supervision to monitor their heart condition.
CNS metastases
The efficacy and safety of Abraxane in patients with CNS metastases has not been determined. Typically, metastases to the CNS are poorly controlled by systemic chemotherapy.
Gastrointestinal symptoms
If nausea, vomiting and diarrhea occur during treatment with Abraxane, patients may be prescribed standard antiemetics and anti-diarrheals.
Elderly patients 75 years of age and older
In patients 75 years of age and older, no benefit of combination therapy with Abraxane and gemcitabine compared to gemcitabine monotherapy was noted.
In very elderly patients (â¥75 years of age), an increased incidence of serious NLDs and NLDs leading to early termination of therapy, including hematologic toxicity, peripheral neuropathy, decreased appetite and dehydration were noted on combination therapy with Abraxane and gemcitabine.
Pancreatic adenocarcinoma patients aged â¥75 years should be closely monitored to assess the tolerability of combination therapy with Abraxane and gemcitabine.
Particular attention should be paid to their general condition, comorbidities and increased risk of infection.
Other
According to the limited data available, no clear benefit of combination therapy with Abraxane and gemcitabine has been found in terms of increased overall survival in pancreatic adenocarcinoma patients with normal CA 19-9 values prior to treatment initiation.
Erlotinib should not be added to the combination of Abraxane and gemcitabine.
Excipients
After recovery, 1 ml of Abraxane contains 183 mmol or 4.2 mg of sodium. This should be kept in mind for patients on a sodium-restricted diet.
Abraxan is an albumin-stabilized nanodispersed paclitaxel whose pharmacological properties may differ substantially from those of other paclitaxel drugs. Do not use together with or in place of other dosage forms of paclitaxel.
The concentration of the ready-to-use suspension is 5 mg/ml, do not dilute before administration!
Precaution
The rules for handling and destroying cytotoxic substances must be followed when working with Abraxane.
The preparation must be prepared for administration by specially trained personnel in a room with aseptic conditions. The use of protective gloves, goggles and protective clothing is recommended.
Contact of the drug with skin and mucous membranes should be avoided. If the drug comes into contact with the skin, the affected area should be immediately washed thoroughly with soap and water. A tingling/burning sensation and reddening of the skin may occur.
In case of contact of the drug Abraxane with the mucous membranes the affected area should be thoroughly rinsed with water. Inhalation of paclitaxel may cause shortness of breath, chest pain, burning sensation in the eyes, sore throat and nausea.
Pregnant female employees should not work with Abraxane.
Impact on driving and operating ability
Abraxan has a slight to moderate effect on driving and operating ability.
At the same time, Abraxane is capable of causing adverse reactions, particularly fatigue (very common) and dizziness (common), which may affect patients’ ability to drive and operate vehicles.
Patients should be advised to refrain from driving vehicles and operating machinery if fatigue or dizziness develops.
Contraindications
Contraindications
Side effects
Side effects
The most frequent and clinically significant NCDs developing during treatment with Abraxane were neutropenia, peripheral neuropathy, arthralgia/myalgia and gastrointestinal disorders.
The following describes the NLDs reported with Abraxane as monotherapy and in combination with gemcitabine for all possible indications.
Definition of the incidence of NLD: very common (â¥1/10), common (< 1/10-â¥1/100), infrequent (< 1/100-â¥1/1000), rare (< 1/1000-â¥1/10 000), very rare (< 1/10 000).
Breast cancer (Abraxane monotherapy)
Infectious and parasitic diseases:
often – infections, urinary tract infections, folliculitis, upper respiratory tract infections, candidiasis, sinusitis;
infrequent – oral candidiasis, nasopharyngitis, phlegmon, herpes simplex, viral infections, pneumonia, catheter-associated infections, fungal infections, shingles, injection site infectious complications, sepsis, neutropenic sepsis.
Benign, malignant and unspecified neoplasms (including cysts and polyps):
Blood and lymphatic system disorders:
Immune system disorders:
Metabolic and nutritional side:
Mental disorders:
Nervous system disorders:
Overdose
Overdose
Treatment: The specific antidote for paclitaxel is unknown. In case of overdose of Abraxane, symptomatic treatment and close monitoring of the patient are carried out. Treatment should be aimed at the main predictable complications (myelosuppression, mucositis and peripheral neuropathy).
Pregnancy use
Pregnancy use
Pregnancy
There are limited data on the use of paclitaxel in pregnant women. It is assumed that when administered during pregnancy paclitaxel causes severe birth defects. Animal studies have shown reproductive toxicity of the drug. The use of the drug Abraxane in pregnancy is contraindicated.
Women of childbearing age should use reliable contraception.
Breast-feeding period
It is unknown whether paclitaxel passes into breast milk. Given the possible serious adverse reactions in breastfed children, Abraxane is contraindicated for breastfeeding women. Women treated with Abraxane should stop breastfeeding.
Fertility
In in vivo studies, paclitaxel has been found to have genotoxic, teratogenic, embryo and fetotoxic effects and decreases reproductive function in both males (testicular atrophy/degeneration) and females (reduced pregnancy rates and increased fetal death).
Additional information
| Weight | 0.088 kg |
|---|---|
| Manufacturer | Abraxis BioScience LLC, USA |
| Medication form | lyophilizate |
| Brand | Abraxis BioScience LLC |
Related products
Buy Abraxane, lyophilizate 100 mg with delivery to USA, UK, Europe and over 120 other countries.